Intermittent Catheters
- Written by: Diane K. Newman, DNP, ANP-BC, FAAN
- References:
- Beauchemin, L. , Newman, D.K., Le Danseur, M., Jackson,A., &Ritmiller, M. (2018). Best practices for clean intermittent catheterization. 48(9): 49-54
- Bhatt, N. R., Davis, N. F., Thorman, H., Brierly, R., & Scopes, J. (2021). Knowledge, skills, and confidence among healthcare staff in urinary catheterization. Canadian Urological Association Journal, 15(9). https://doi.org/10.5489/cuaj.6986
- Goetz, L.L., Droste, L., Klausner, A.P., & Newman, D.K. (2018). Intermittent catheterization. In: D.K. Newman, E.S. Rovner, A.J. Wein, (Eds). Clinical Application of Urologic Catheters and Products. (pp. 47-77) Switzerland: Springer International Publishing. Moore, KN., Fader, M. & Getliffe, K. Long‐term bladder management by intermittent catheterisation in adults and children. Cochrane Database of Systematic Reviews4 (2007).
- Hakansson MA. (2014). Reuse versus single-use catheters for intermittent catheterization: what is safe and preferred? Review of current status. Spinal Cord. 52:511–6.
- Sun AJ, Comiter CV, Elliott CS. (2018). The cost of a catheter: an environ- mental perspective on single use clean intermittent catheterization. Neurourol Urodyn. 37:2204–8.
- van Doorn, T.Bertil F M Blok, BFM. (2020). Multiuse Catheters for Clean Intermittent Catheterization in Urinary Retention: Is There Evidence of Inferiority? Eur Urol Focus. 15;6(5):809-810. doi: 10.1016/j.euf.2019.09.018.
- Walter, M, & Krassioukov, A.V. (2020). Single-use Versus Multi-use Catheters: Pro Single-use Catheters. Eur Urol Focus. 6(5):807-808. doi: 10.1016/j.euf.2019.10.001.
Best Practices for Management - Intermittent Catheters

Patients may be concerned about the discomfort associated with intermittent catheterization(IC), the need to maintain privacy, the fear of performing the catheterization, and the inability to find a clean and appropriate toilet or bathroom for catheterization when traveling outside their home. Clinicians need to consider these patient concerns in their teaching and recommend possible strategies.
Teaching Catheterization:
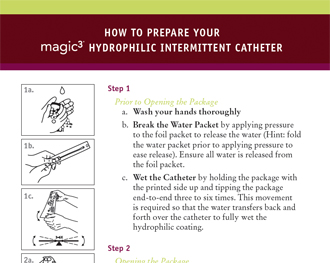
Successful intermittent self-catheterization (ISC) requires education and support, particularly during initial teaching and follow up. Although long term ISC is safe and well accepted, an early dropout rate of about 20% has been described in children and adolescents (Pohl et al., 2002), so good support, professional instruction on catheterization technique and periodic follow-up is necessary to obtain and maintain patient compliance. A knowledgeable and experienced clinician, in most cases a nurse, is an important component for successful self-catheterization teaching. The nurse should assess what the patient and/or the person performing the catheterization knows about the urinary tract and functions of the bladder. Providing an overview of anatomy with pictures or the use of an anatomic model of the perineum can be very helpful. Many catheter manufacturers have visual guides or videos that can be used when teaching patients and/or caregivers.
Other teaching components include how to handle the catheter, identifying the urinary meatus, and care of the catheter. It is important that patients and/or the person performing the catheterization demonstrate understanding and/or ability or perform catheterization under the supportive supervision of the nurse.
Teaching Environment:
Most adults learn best under low to moderate stress, so it is important to teach self-catheterization in a low stress setting. The nurse should also assess the patient’s ability to learn intermittent self-catheterization (ISC), motivation to continue long-term catheterization, awareness of problems associated with catheterization, and the understanding of how to avoid possible complications. Other factors to consider are the patient’s bladder capacity (still voiding some amounts or complete retention), adequate bladder outlet resistance (absence of urethral scarring, strictures or enlarged prostate), absence of urethral sensitivity to pain with catheterization, and patient’s possible fear of catheterization. Initially, many patients may be extremely reluctant to perform any procedure that involves the genitals, but this is basically a “fear of the unknown.” Determining acceptance of intermittent catheterization is vital because non-compliance is seen in many patients, particularly adolescents.
General Assessment:
Many clinicians are concerned about teaching an older patient ISC but age is not necessarily a determinant to the success of ISC. Disabilities, such as poor eyesight or blindness, poor hand dexterity, lack of perineal sensation, tremor, mental disability, and paraplegia, do not necessarily preclude the ability to perform ISC. But these obstacles may be difficult to overcome in some patients and caregivers. Teaching a patient with a spinal cord injury maybe even more of a challenge because motor and sensory impairment may require changes to catheterization techniques. Impaired cognitive function can affect success in being able to carry out the procedure independently.
Important Medical History:
Any previous experience with catheterization (e.g indwelling or IC) should be determined prior to teaching a patient ISC as this will direct the teaching and should be considered when choosing a catheter. In a male patient, a history of urethral strictures or scarring or enlarged prostate may indicate need for a Coudé tip catheter. If a woman has pelvic organ prolapse, angling the catheter around the prolapse may be needed.
Choosing the catheter:
With advances in catheter technology, the number of catheter types and designs has increased, adding complexity to the catheterization process for both the nurse and the patient. Catheter types are now gender specific, long length for males, shorter length for females. acknowledging the anatomical differences in urethral length between men and women.
Design changes include the integration of all needed equipment (such as catheter, water-based
lubricant, and drainage bag) into a compact and user friendly system. These are referred to as “closed systems or kits”. But some patients with limited dexterity may find it difficult to advance a catheter through a collection bag.

When recommending a catheter, consider the patient’s lifestyle including plans for catheter storage, carrying, and disposal. Offering a selection of three to four types of catheter is recommended.
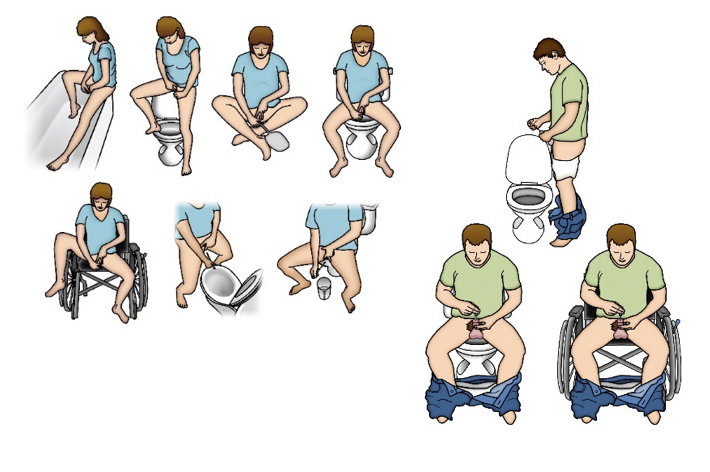
Catheterization Position:
IC teaching includes identifying the best position for performing catheterization and it should be individualized for each patient. Variables to consider when assessing a patient for the ideal position includes abnormally high body mass index and body hiatus (large pannus) as both could restrict perineal and urethral access. Most patients tend to catheterize in their bathroom, sitting on or standing in front of a toilet. For someone who is in a wheelchair most of the day, catheterizing while sitting in the chair is an option but maybe more difficult for women. Women may choose to use a mirror to visualize the urethra is also an option.
Catheterization Schedule:
The frequency of catheterization depends on patient history and the clinical reasons for initiating an IC program: for example, the individual with reflux and symptomatic UTI will require more frequent catheterizations than the person who is using IC to manage leakage caused by incomplete emptying and who has no UTI symptoms. A catheterization schedule can be recommended based on frequency-volume records, functional bladder capacity based on urodynamics findings, ultrasound bladder scans for PVR, and the impact of catheterization on a patient’s quality of life. As a general rule, bladder volume should not exceed 500 mLs, and some advocate not exceeding 400 mLs. Based on an individual’s average output, catheterization is usually performed four to six times during the day. Many patients, especially older patients, may need to catheterize at bedtime and during the night. The bladder should be emptied completely with each catheterization. When starting intermittent catheterization, the patient and/or caregiver should record the amount of urine drained from the bladder. If the patient voids, catheterization should always be performed after voiding.
Catheter Use and Care:
 recommended. The cleaning of the catheter between uses has no basis in research because there are no published randomized controlled clinical trials of cleaning methods. The comparative effectiveness of cleaning methods, therefore, is unknown.
recommended. The cleaning of the catheter between uses has no basis in research because there are no published randomized controlled clinical trials of cleaning methods. The comparative effectiveness of cleaning methods, therefore, is unknown.Currently, catheter manufacturers do not provide instructions for catheter re-use or cleaning. So best practices do not support the re-use of single-use catheters at this time.
There are no set guidelines for monitoring patients performing ISC, although many urologists advocate regular urine cytology and cystoscopy with random or targeted bladder biopsies.
In reality, many patients performing intermittent catheterization are lost to urologic follow up.
March 2021
© 2021 Digital Science Press, Inc. and UroToday.com
- Written by: Diane K. Newman, DNP, ANP-BC, FAAN
- References:
- Beauchemin L, Newman DK, Le Danseur M, Jackson A, Ritmiller M. (2018). Best practices for clean intermittent catheterization. 48, 9(Sept 2018):49-54.
- Canadian Practice Recommendations For Nurses, Clean Intermittent Urethral Catheterization in Adults, (April, 2020), Retrieved from: https://ipac-canada.org/photos/custom/Members/pdf/Clean-Intermittent-Urethral-Catheterization-Adults-for-Nurses-BPR-May2020.pdf
- Gray, M., Wasner, M., Nichols, T.J. (2019). NursingPractice Related to IntermittentCatheterization: A Cross-Sectional Survey. Wound Ostomy Continence Nurs. 46(5):418-423. doi: 10.1097/WON.0000000000000576.
- Goetz, L.L., Droste, L., Klausner, A.P., & Newman, D.K. (2018). Intermittent catheterization. In: D.K. Newman, E.S. Rovner, A.J. Wein, (Eds). Clinical Application of Urologic Catheters and Products. (pp. 47-77) Switzerland: Springer International Publishing.
- Hentzen, C., Haddad, R., Ismael, S.S., Peyronnet, B., Gamé, X., Denys, P., … GRAPPPA (Clinical research Group of perineal dysfunctions in older adults). (2018) Intermittent self-catheterization in older adults: predictors of success for technique learning. Int Neurourol J. 22(1):65‐ https://doi.org/10.5213/inj.1835008.504
- Logan, K. (2020). An exploration of men's experiences of learning intermittent self-catheterisation with a silicone catheter. Br J Nurs. 29(2):84-90. https:// doi: 10.12968/bjon.2020.29.2.84
- Logan, K. (2017). The female experience of ISC with a silicone catheter. Br J Nurs. 26(2):82-88. https://doi: 10.12968/bjon.2017.26.2.82.
- Logan, K. (2015). The male experience of ISC with a silicone catheter. Br J Nursing 24(9), S32–4. https://doi: 10.12968/bjon.2015.24.Sup9.S30.
- Mangnall, J. (2015) Managing and teaching intermittent catheterisation. Br J Community Nurs. 20(2):82. https://doi.org/10.12968/bjcn.2015.20.2.82
- Martins, G., Soler, Z.A., Batigalia, F., & Moore, K.N. (209). Clean intermittent catheterization: Educational booklet directed to caregivers of children with neurogenic bladder dysfunction. Journal Wound Ostomy Conti. N, 36(5), 545-549.
- Newman DK. (2017). Devices, products, catheters, and catheter-associated urinary tract infections. In: Newman DK, Wyman JF, Welch VW, editors. Core Curriculum for Urologic Nursing. 1st Pitman (NJ): Society of Urologic Nurses and Associates, Inc; 439-66.
- Newman DK, Willson MM. (2011) Review of intermittent catheterization and current best practices. Urol Nurs. Jan-Feb;31(1):12-28, 48; quiz 29. PubMed PMID: 21542441
- Pohl, H.G., Bauer, S.B., Borer, J.G., Diamond, D.A., Kelly, M.D., Grant, R., ... Retik, A.B.. (2002). The outcome of voiding dysfunction managed with clean intermittent catheterization in neurologically and anatomically normal children. British Journal of Urology International, 89(9), 923-927.
- Vahr, S., Cobussen-Boekhorst, H., Eikenboom, J., Geng, V., Holroyd, S., Lester, M., … Vandewinkel, C. (2013). Evidence-based guidelines for best practice in urological health care catheterisation dilatation, urethral intermittent in adults. European Association of Urology Nurses. Retrieved from http://nurses.uroweb.org/wpcontent/uploads/2013_EAUN_Guide line_Milan_2013-Lr_DEF.pdf
- Vahr, S., Cobussen-Boekhorst, H., Eikenboom, J., Geng, V., Holroyd, S., Lester, M., … Vandewinkel, C. members of the European Association of Urology Nurses Guidelines Office. An edited summary of the European Association of Urology Nurses evidence-based guideline on Intermittent Urethral Catheterisation in Adults – Evidence-based Guidelines for Best Practice in Urological Health Care. Edition presented at the 18th International EAUN Meeting, London 2017. ISBN 978-90-79754-92-2. Retrieved from http://www.eaun.uroweb.org
- Woodbury M.G., Hayes K.C., & Askes H.K. (2008). Intermittent catheterization practices following spinal cord injury: A national survey. Canadian Journal Urology, 15(3), 4065-4071.
Indication of Catheterization for Intermittent Catheters (IC)
- Written by: Diane K. Newman, DNP, ANP-BC, FAAN
- References:
- Apostolidis, A., Drake, M., Emmanuel, A., Gajewski, J., Heesakkers, J., Kessler, T., …..Wyndaele, J.J. (2017) Neurologic urinary and fecal urinary incontinence. In: P. Abrams P CL, L.Cardozo, A. Wagg, A.Wein (Eds). International Consultation on Incontinence 6th edition. (pp. 1093-1308). Plymouth, UK: Health Publications Ltd.
- Averch, T.D., Stoffel, J., Goldman, H.B., Griebling, T., Lerner, L., Newman, D.K., Peterson, A.C. (2014) AUA White Paper on Catheter-Associated Urinary Tract Infections: Definitions and Significance in the Urologic Patient Workgroup, Retrieved from https://www.sciencedirect.com/science/article/pii/S2352077915000308
- Blok B, J. P-F, Pannek J, Castro-Diaz D, Del Popolo G, Groen J, Hamid R, Karsenty G, Kessler TM (2018) Guidelines on Neuro-Urology. EAU European Association of Urology, Retrieved from https://uroweb.org/wp-content/uploads/EAU-Guidelines-on-Neuro-Urology-2018-large-text.pdf
- Bladder management following spinal cord injury. Spinal cord injury rehabilitation evidence. 2014. https://msktc.org/lib/docs/Factsheets/SCI_Bladder_Health.pdf Accessed March 18, 2021
- Cottenden, A., Fader, M., Beeckman, D., Buckley, B., Kitson-Reynolds, E., Moore, K…..Wilde, M. (2017) Management using continence products. In: P. Abrams P CL, L.Cardozo, A. Wagg, A.Wein (Eds). International Consultation on Incontinence 6th edition. (pp. 2303-2426). Plymouth, UK: Health Publications Ltd
- Gajewski, J.B., Schurch B, Hamid R, Averbeck, A., Sakakibara, R., Agro, E.F.,…Haylen, B.T. (2018). An International Continence Society (ICS) report on the terminology for adult neurogenic lower urinary tract dysfunction (ANLUTD). Neurourology and Urodynamics, 37:1152–1161. https://doi.org/10.1002/nau.23397
- Gamé X, Phé V, Castel-Lacanal E, Forin V, de Sèze M, Lam O, Chartier-Kastler E, Keppenne V, Corcos J, Denys P, Caremel R, Loche CM, Scheiber-Nogueira MC, Karsenty G, Even A. (2020). Intermittent catheterization: Clinical practice guidelines from Association Française d'Urologie (AFU), Groupe de Neuro-urologie de Langue Française (GENULF), Société Française de Médecine Physique et de Réadaptation (SOFMER) and Société Interdisciplinaire Francophone d'UroDynamique et de Pelvi-Périnéologie (SIFUD-PP). Prog Urol. Mar 24. pii: S1166-7087(20)30054-3. doi: 10.1016/j.purol.2020.02.009
- Ginsberg D. (2013). The epidemiology and pathophysiology of neurogenic bladder. Am J Manag Care. 2013;19(10 suppl):s191-6. http://www.ncbi.nlm. nih.gov/pubmed/24495240
- Groen J, Pannek J, Castro Diaz D, Del Popolo G, Gross T, Hamid R, Karsenty G, Kessler TM, Schneider M, Hoen L, Blok B. (2016) Summary of European Association of Urology(EAU) Guidelines on Neuro-Urology. Eur Urol. 69(2):324-33. doi: 10.1016/j.eururo.2015.07.071
- Goetz, L.L., Droste, L., Klausner, A.P., & Newman, D.K. (2018). Intermittent catheterization. In: D.K. Newman, E.S. Rovner, A.J. Wein, (Eds). Clinical Application of Urologic Catheters and Products. (pp. 47-77) Switzerland: Springer International Publishing.
- Gould, C., Umscheid, C., Agarwal, R., et al.; Healthcare Infection Control Practices Advisory Committee (HICPAC). (2009). In Guideline for prevention of catheter-associated urinary tract infections. Atlanta, GA: Centers for Disease Control and Prevention (CDC). Retrieved from http://www.cdc.gov/hicpac/pdf/cauti/cautiguideline2009final.pdf
- Gould CV, Umscheid CA, Agarwal RK, Kuntz G, Pegues DA (2010) Guideline for prevention of catheter-associated urinary tract infections 2009. Infection control and hospital epidemiology : the official journal of the Society of Hospital Epidemiologists of America. 31(4):319-326. doi:10.1086/651091
- Kennelly M, Thiruchelvam N, Averbeck MA, Konstatinidis C, Chartier-Kastler E, Trøjgaard P, Vaabengaard R, Krassioukov A, Jakobsen BP. AdultNeurogenic LowerUrinary Tract Dysfunction and Intermittent Catheterisation in a Community Setting: Risk Factors Model for Urinary Tract Adv Urol. 2019 Apr 2;2019:2757862. doi: 10.1155/2019/2757862.
- Kinnear, N., Barnett, D., O'Callaghan, M., Horsell, K., Gani, J, Hennessey, D. (2020). The impact of catheter-based bladder drainage method on urinary tract infection risk in spinal cord injury and neurogenic bladder: A systematic review. Neurourol Urodyn. 39(2):854-862. doi: 10.1002/nau.24253
- Klausner, A.P., & Steers, W.D. (2011). The neurogenic bladder: an update with management strategies for primary care physicians. Med Clin North Am. 95(1):111-20. https://DOI: 10.1016/j.mcna.2010.08.027.
- Lavis T, Goetz LL. (2019) Comprehensive care for persons with spinal cord injury. Phys Med Rehabil Clin N Am. 30(1):55-72. doi:10.1016/j.pmr.2018.08.010
- Management of the neurogenic bladder for adults with spinal cord injuries. https://www.aci.health.nsw. gov.au/__data/assets/pdf_file/0010/155179/ Management-Neurogenic-Bladder.pdf Accessed March 20, 2021
- Milligan J, Goetz LL, Kennelly MJ. (2020). A Primary Care Provider's Guide to Management of Neurogenic Lower UrinaryTractDysfunction and Urinary Tract Infection After Spinal Cord Injury. Top Spinal Cord Inj Rehabil. Spring;26(2):108-115. doi: 10.46292/sci2602-108
- Newman, D.K. (2017). Devices, products, catheters, and catheter-associated urinary tract infections. In: D.K. Newman, J.F. Wyman, V.W. Welch (Eds). Core Curriculum for Urologic Nursing (pp. 429-466). Pitman, New Jersey: Society of Urologic Nurses and Associates, Inc.
- Newman, D.K., & Wein, A.J. (2009). Managing and treating urinary incontinence (2nd ed). Baltimore: Health Professions Press.
- Panicker JN. (2020) NeurogenicBladder: Epidemiology, Diagnosis, and Management. Semin Neurol. Oct;40(5):569-579. doi: 10.1055/s-0040-1713876.
- Tate DG, Wheeler T, Lane GI, Forchheimer M, Anderson KD, Biering-Sorensen F, Cameron AP, Santacruz BG, Jakeman LB, Kennelly MJ, Kirshblum S, Krassioukov A, Krogh K, Mulcahey MJ, Noonan VK, Rodriguez GM, Spungen AM, Tulsky D, Post MW. Recommendations for evaluation of neurogenicbladderand bowel dysfunction after spinal cord injury and/or disease. J Spinal Cord Med. 2020 Mar;43(2):141-164. doi: 10.1080/10790268.2019.1706033
Intermittent Catheter Types
- Written by: Diane K. Newman, DNP, ANP-BC, FAAN
- References:
- Chartier-Kastler E, Amarenco G, Lindbo L, et al. (2013). A prospective, randomized, crossover, multicenter study comparing quality of life using compact versus standard catheters for intermittent self-catheterization. J Urol. 190(3):942-947.
- Cardenas, D. D., Moore, K. N., Dannels-McClure, A., et al. (2011). Intermittent catheterization with a hydrophilic-coated catheter delays urinary tract infections in acute spinal injury: A prospective randomised, multicenter trial. Physical Medicine and Rehabilitation, 3(5), 408–417.
- Christnsen, J., Ostri, P., Frimodt-moller, C., et al. (1987). Intravesical pressure changes during bladder drainage in patients with acute urinary retention. Urologia Internationalis, 42(3), 181–184.
- Christison K, Walter M, Wyndaele JJM, et al. (2018). Intermittent catheterization: The devil is in the details. J Neurotrauma. Feb 1. doi: 10.1089/neu.2017.5413doi
- DeFoor W, Reddy P, Reed M, et al. (2017). Results of a prospective randomized control trial comparing hydrophilic to uncoated catheters in children with neurogenic bladder. J Pediatr Urol. Aug;13(4):373.e1-373.e5. doi: 10.1016/j.jpurol.2017.06.003.
- Goetz LL, Droste L, Klausner AP, Newman DK. (2018). Intermittent catheterization. In: D.K. Newman, E.S. Rovner, A.J. Wein, (Eds). Clinical Application of Urologic Catheters and Products. (pp. 47-77) Switzerland: Springer International Publishing
- Håkansson MA. (2014). Reuse versus single-use catheters for intermittent catheterization: what is safe and preferred? Review of current status. Spinal Cord. 52(7):511-516.
- Newman, D.K., New, P.W., Heriseanu, R. Petronis, S., Håkansson, J., Håkansson, M.A., & Lee, B.B. (2020). Intermittent catheterization with single- or multiple-reuse catheters: clinical study on safety and impact on quality of life. Int Urol Nephrol. Aug;52(8):1443-1451. doi: 10.1007/s11255-020-02435-9.
- Newman DK. (2017). Devices, products, catheters, and catheter-associated urinary tract infections. In: Newman DK, Wyman JF, Welch VW, editors. Core Curriculum for Urologic Nursing. 1st Pitman (NJ): Society of Urologic Nurses and Associates, Inc; 2017. p.439-66.
- Newman DK, Willson MM. (2011). Review of intermittent catheterization and current best practices. Urol Nurs. Jan-Feb;31(1):12-28, 48; quiz 29. PubMed PMID: 21542441
- Rognoni C, Tarricone R. (2017). Intermittent catheterization with hydrophilic and non-hydrophilic urinary catheters: systematic literature review and meta-analyses. BMC Urol. 17(1):4.
- Shamout S, Biardeau X, Corcos J, Campeau L. (2017). Outcome comparison of different approaches to self-intermittent catheterization in neurogenic patients: a systematic review. Spinal Cord. 55(7):629-643.
- Sun AJ, Comiter CV, Elliott CS. (2018). The cost of a catheter: An environmental perspective on single-use clean intermittent catheterization. Neurourol Urodyn. 37(7):2204-2208.
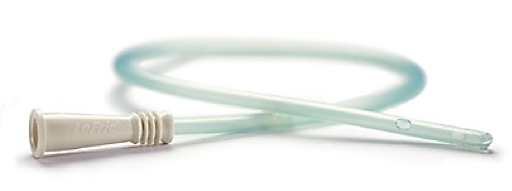
Definition - Intermittent Catheters
What is an intermittent urinary catheter?
Intermittent catheterization (IC) is the insertion and removal of a catheter several times a day to empty the bladder. The purpose of catheterization is to drain urine from a bladder that is not emptying adequately or from a surgically created channel that connects the bladder with the abdominal surface (such as Mitrofanoff continent urinary diversion).
Intermittent catheterization is widely advocated as an effective bladder management strategy for patients with incomplete bladder emptying due to idiopathic or neurogenic detrusor (bladder) dysfunction (NDO).
- Written by: Diane K. Newman, DNP, ANP-BC, FAAN
- References:
- Averbeck MA, Krassioukov A, Thiruchelvam N, Madersbacher H, Bogelund M, Igawa Y. The impact of different scenarios for intermittent bladder catheterization on health state utilities: results from an internet-based time trade-off survey. J Med Econ. 2018:1-8.
- Avery M, Prieto J, Okamoto I, et al. Reuse of intermittent catheters: a qualitative study of IC users' perspectives. BMJ open. 2018;8(8):e021554
- Beauchemin L, Newman DK, Le Danseur M, Jackson A, Ritmiller M. Best practices for clean intermittent catheterization. Nursing. 2018;48(9):49-54.
- DeFoor W, Reddy P, Reed M, et al. Results of a prospective randomized control trial comparing hydrophilic to uncoated catheters in children with neurogenic bladder. J Pediatr Urol. 2017;13(4):373.e371–373.e375.
- Goetz LL, Droste L, Klausner AP, Newman DK. Catheters Used for Intermittent Catheterization. Clinical Application of Urologic Catheters, Devices and Products. Cham: Springer International Publishing; 2018:47-77.
- Heard, L. & Buhrer, R. How do we prevent UTI in people who perform intermittent catheterization? Rehabilitation Nursing, 2005: (30): p 44–45.
Krassioukov A, Cragg JJ, West C, Voss C, Krassioukov-Enns D. The good, the bad and the ugly of catheterization practices among elite athletes with spinal cord injury: a global perspective. Spinal Cord. 2015;53(1):78-82. - Lapides, J., Diokno, A.C., Silber, S.J., & Lowe, B.S., Clean, intermittent self-catheterization in the treatment of urinary disease. 1972. Urology:107; p458.
- Lapides, J., Diokno, A.C., Silber, S.M., & Lowe, B.S. Clean, intermittent self-catheterization in the treatment of urinary tract disease. 1972. Journal of Urology: 167; p1584–1586.
- Newman DK. (2017). Devices, products, catheters, and catheter-associated urinary tract infections. In: Newman DK, Wyman JF, Welch VW, editors. Core Curriculum for Urologic Nursing. 1st ed. Pitman (NJ): Society of Urologic Nurses and Associates, Inc; 439-66.
- Newman DK, Willson MM. Review of intermittent catheterization and current best practices. Urol Nurs. 2011 Jan-Feb;31(1):12-28, 48; quiz 29. PubMed PMID: 21542441
11. Vahr S, Cobussen-Boekhorst H, Eikenboom J, et al. Evidence-based guideline for best practice in urological health care. Catheterization. Urethral intermittent in adults. Dilatation, urethral intermittent in adults. . EAUN guideline. 2013.
Video Lectures - Intermittent Catheters
The following lecture series is presented by:
Diane K. Newman, DNP, ANP-BC, FAAN
Adjunct Associate Professor of Urology in Surgery
Research Investigator Senior
Perelman School of Medicine, University of Pennsylvania
Co-Director, Penn Center for Continence and Pelvic Health
Division of Urology, University of Pennsylvania Health System
Philadelphia, PA
Click on any image to watch
|
|
||||
|
|
||||
|
|||||
Complications - Intermittent Catheters
Urethral Adverse Events | Scrotal Complications | Bladder-related Complications | Pain | Urinary Tract Infections | Causes of IC-related UTIs | Video Lecture | References
Intermittent catheterization (IC) is the preferred procedure for individuals with incomplete bladder emptying from non-neurogenic or neurogenic lower urinary tract dysfunction (NLUTD). IC is now considered the gold standard for bladder emptying in individuals following spinal cord injury (SCI) who have sufficient manual dexterity (Groen et al., 2016; Wyndaele et al, 2012). Goals of bladder management in individuals with a SCI include prevention of infection, injuries or trauma, optimizing social continence and function, and preventing upper tract deterioration. Despite these recommendations, complications and adverse events can arise in both men and women but are seen especially in male patients performing intermittent self-catheterization (ISC) for long-term.
- Written by: Diane K. Newman, DNP, ANP-BC, FAAN
- References:
- Bailey, L. & Jaffe, W.I. (2017). Obstructuve uropathy. In: D.K. Newman, J.F. Wyman, V.W. Welch, (Eds). Core Curriculum for Urologic Nursing. (pp.405-421) Pitman, New Jersey: Society of Urologic Nurses and Associates, Inc.
- Casey, R.G., Cullen I.M., Crotty, T., & Quinlan, D.M. (2009) Intermittent self-catheterization and the risk of squamous cell cancer of the bladder: An emerging clinical entity? Canadian Urological Association Journal, 3(5), E51-E54.
- Clarke, S.A., Samuel, M., & Boddy, S.A. (2005). Are prophylactic antibiotics necessary with clean intermittent catheterization? A randomized controlled trial. Journal of Pediatric Surgery, 40, 568-571.
- Cornejo-Davila V, Duran-Ortiz S, Pacheco-Gahbler C. (2017). Incidence of urethral stricture in patients with spinal cord injury treated with clean intermittent self-catheterization. Urology. 99:260–4.
- Cortese YJ, Wagner VE, Tierney M, Scully D, Devine DM, Fogarty A. (2020). Pathogen displacement during intermittent catheter insertion: a novel in vitro urethra model. J Appl Microbiol. Apr;128(4):1191-1200. doi: 10.1111/jam.14533.
- Cox L, He C, Bevins J, Clemens JQ, Stoffel JT, Cameron AP. (2017). Gentamicin bladder instillations decrease symptomatic urinary tract infections in neurogenic bladder patients on intermittent catheterization. Can Urol Assoc J. Sep;11(9):E350-E354. doi: 10.5489/cuaj.4434
- de Avila MAG, Rabello T, de Araújo MPB, Amaro JL, Zornoff DCM, Ferreira ASSBS, de Oliveira AS. (2021). Development and Validation of an Age-Appropriate Website for Children Requiring Clean IntermittentCatheterization. Rehabil Nurs. 2021 Mar-Apr 01;46(2):65-72. doi: 10.1097/rnj.0000000000000253
- De Ridder, D. J. M. K., Everaert, K., Fernandez, L. G., et al. (2005). Intermittent catheterisation with hydrophilic-coated catheters (SpeediCath) reduces the risk of clinical urinary tract infection in spinal cord injured patients: A prospective randomized parallel comparative trial. European Urology, 48(6), 991–995
- Groen J, Pannek J, Castro Diaz D, Del Popolo G, Gross T, Hamid R, et al. (2016). Summary of European Association of Urology (EAU) Guidelines on Neuro-Urology. Eur Urol. 69:324–33.
- Kinnear, N., Barnett, D., O'Callaghan, M., Horsell, K., Gani, J, Hennessey, D. (2020). The impact of catheter-based bladder drainage method on urinary tract infection risk in spinal cord injury and neurogenic bladder: A systematic review. Neurourol Urodyn. 39(2):854-862. doi: 10.1002/nau.24253
- Marei MM, Jackson R, Keene DJB. (2021). Intravesical gentamicin instillation for the treatment and prevention of urinarytract infections in complex paediatric urology patients: evidence for safety and efficacy. J Pediatr Urol. 17(1):65.e1-65.e11. doi: 10.1016/j.jpurol.2020.08.007
- Mitchell BG, Prael G, Curryer C, Russo PL, Fasugba O, Lowthian J, Cheng AC, Archibold J, Robertson M, Kiernan M. (2021). The frequency of urinarytract infections and the value of antiseptics in community-dwelling people who undertake intermittent urinarycatheterization: A systematic review. Am J Infect Control. Jan 21:S0196-6553(21)00022-5. doi: 10.1016/j.ajic.2021.01.009
- Moussa M, Chakra MA, Papatsoris AG, Dellis A, Dabboucy B, Fares Y. (2021). Bladder irrigation with povidone-iodine prevent recurrent urinarytract infections in neurogenic bladder patients on clean intermittent catheterization. Neurourol Urodyn. Feb;40(2):672-679. doi: 10.1002/nau.24607. Epub 2021 Jan 21
- Newman, D.K., New, P.W., Heriseanu, R. Petronis, S., Håkansson, J., Håkansson, M.A., & Lee, B.B. (2020). Intermittent catheterization with single- or multiple-reuse catheters: clinical study on safety and impact on quality of life. Int Urol Nephrol. Aug;52(8):1443-1451. doi: 10.1007/s11255-020-02435-9.
- Patel DP, Herrick JS, Stoffel JT, et al. (2020) Reasons for cessation of clean intermittent catheterization after spinal cord injury: Results from the Neurogenic Bladder Research Group spinal cord injury registry. Neurourology and Urodynamics. 39:211–https://doi.org/10.1002/nau.24172
- Stensballe, J., Loom, D., et al. (2005). Hydrophilic-coated catheters for intermittent catheterisation reduce urethral microtrauma: A prospective, randomised, participant blinded, crossover study of three different types of catheters. Eu Urol, 48, 978-983.
- Stillman MD, Hoffman JM, Barber JK, Williams SR, Burns SP. (2018). Urinary tract infections and bladder management over the first year after discharge from inpatient rehabilitation. Spinal Cord Ser Cases. Oct 19;4:92. doi: 10.1038/s41394-018-0125-0.
- Stohrer M, Blok B, Castro-Diaz D, Chartier-Kastler E, Del Popolo G, Kramer G, Pannek J, Radziszewski P, Wyndaele JJ. (2009). EAU guidelines on neurogenic lower urinary tract dysfunction. Eur Urol. 56:81--8. doi: 10.1016/j.eururo.2009.04.028.
- Vapnek, J.M., Maynard, F.M., & Kim, J. (2003). A prospective randomized trial of the LoFric hydrophilic coated catheter versus conventional plastic catheter for clean intermittent catheterization. Journal of Urology.169, 994-998.
- Walter, M., Ruiz, I. Squair, JW., Rios, LAS., Averbeck, MA., Krassioukov, AV. (2020). Prevalence of self-reported complications associated with intermittent catheterization in wheelchair athletes with spinal cord injury. Spinal Cord. Oct 13. doi: 10.1038/s41393-020-00565-6.
- Wyndaele JJ, Brauner A, Geerlings SE, Bela K, Peter T, Bjerklund-Johanson TE. (2012). Clean intermittent catheterization and urinary tract infection: review and guide for future research. BJU Int. 110:E910–7.
- Wyndaele, J.J. (2002). Complications of intermittent catheterization: Their prevention and treatment. Spinal Cord, 40(10), 536-541.
Education Tools - Intermittent Catheters
The following tools are available for download to support patient education for the Magic3® Intermittent Catheter:
|
|
|
|
|
The following tools are available for download to support patient education for the TOUCHLESS® Plus Intermittent Catheter System:
|
|
Published Date: January 31st, 2013