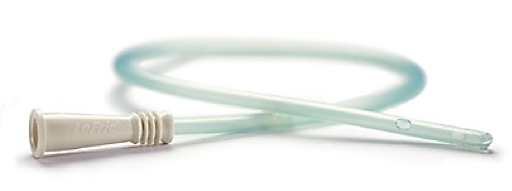
What is an intermittent urinary catheter?
Intermittent catheterization (IC) is the insertion and removal of a catheter several times a day to empty the bladder. The purpose of catheterization is to drain urine from a bladder that is not emptying adequately or from a surgically created channel that connects the bladder with the abdominal surface (such as Mitrofanoff continent urinary diversion).
Intermittent catheterization is widely advocated as an effective bladder management strategy for patients with incomplete bladder emptying due to idiopathic or neurogenic detrusor (bladder) dysfunction (NDO).
Definition of Intermittent Catheterization Methods
Catheterization is performed by the following methods:
Sterile
The typical technique in hospital environments. A sterile catheterization tray is used that includes:
- Sterile gloves
- Genital disinfection
- Single-use catheters
- Sterile draining collector
Aseptic
The aseptic catheterization method includes:
- Use of sterile gloves
- Disinfection of the genitalia with an antiseptic solution
- Single-use catheter
- No direct manual contact with the catheter (e.g. no touch technique, sterile lubricant, or pre-lubricated catheter.)
Intermittent Self-Catheterization (ISC)
Implies that the patient is catheterizing on a schedule determined by drained bladder volume.
- May include a single-use catheter with a non-antiseptic solution for cleaning hands and perineum, or a multiple use catheter; both are referred to as "clean."
- If the catheter is reused, there is no evidence-based research on the best mehtod for cleaning and storing the catheter between uses.
- If a caregiver (e.g. parent catheterizing a child) is performing the procedure, gloves are used.
No-Touch
The user or caregiver never touches the catheter.
- It's inside a protective sleeve or collection bag (e.g. pre-lubricated gel or hydrophilic).
- Or product packaging may be used to hold the catheter during insertion.
Clean Catheterization
Technique that implies hand washing with soap and water, and cleansing the genitilia only if fecal or other wastes are present.
- Involves reuse of hte same catheter for multiple catheterizations and soaking the catheter in an antiseptic between uses or washing them with soap and water and air drying between uses.
- If a caregiver (e.g. parent catheterizing a child) is performing the procedure, gloves are used.
Clean Intermittent Self-Catheterization (CIC)
There is no benefit to the use of an antiseptic solution for daily periurethral cleansing prior to catheterization. In 1972, Jack Lapides, a Urologist at the University of Michigan, and his colleagues (Dr Ananias Diokno) determined that Clean Intermittent Self-Catheterization (CIC) is a safe and effective alternative method of emptying the bladder. It continues to be used more than forty years later to help protect the kidneys, prevent incontinence and decrease the number of infections a patient may acquire by promoting adequate drainage of the bladder while lowering intravesical pressure. Catheterizations performed in institutions, such as acute and rehabilitation hospitals and nursing homes, are done aseptically.
Reuse Risk of CaUTI
Since Dr Lapides first described CIC, intermittent catheterization has been performed by the patient in the home environment using a clean technique. But re-using IC catheters for multiple catheterizations is no longer the preferred or recommended practice for many reasons. Krassioukov et al 2015 concluded that reuse of catheters is associated with greater risk for catheter-associated urinary tract infection (CaUTI) and primarily occur in developing nations with an average frequency of UTI of 3.5 ± 3 per year as compared to 1.6 ± 2 per year for developed nations. DeFoor et al (2018) concluded that single-use hydrophilic-coated catheters significantly reduces the occurrence of UTI as compared to catheter reuse with uncoated catheters. Also, Averbeck et al. (2018) found that single-use catheters are associated with better health states as compared to catheter re-use. Avery et al. (2018) furthermore describe concerns associated with catheter reuse raised by users. These include concerns about catheter-associated UTIs (CaUTIs), cleaning, preparation, storage, lack of discretion. In April 2008, the Centers for Medicare and Medicaid Services (CMS) of the Department of Health and Human Services, USA eliminated the mandatory reuse of intermittent catheters for outpatients who receive such prescriptions from doctors. In short, no more cleaning and reusing catheters at home for people who self-catheterize. Healthcare professionals use their clinical judgment to determine which technique and type of catheter to use, in conjunction with patient preference. Differential costs and insurance coverage of catheters/techniques may also influence decision-making. So it is now recommended that patient’s who perform intermittent self-catheterization (ISC) not re-use the same catheter for multiple catheterizations.
Rationale for Intermittent Catheterization
The rationale for using Intermittent Catheterization:- The bladder contracts and the pelvic floor muscles relax and the external urinary sphincter opens to allow voiding and the passage of urine through the urethra.
- Normally, after the bladder empties, a small amount of urine may remain in the bladder and this is called the postvoid residual (PVR).
- If the person cannot urinate or empty the bladder completely, the PVR increases and can contribute to CaUTIs, overflow UI, and permanent damage to the bladder and kidneys.
- Research has shown that regular bladder emptying reduces intravesical (in the bladder) pressure and improves blood circulation in the bladder wall, making the bladder mucosa more resistant to infectious bacteria.
- By inserting the catheter several times during the day, episodes of bladder overdistention are avoided.
- In addition, the bladder wall is susceptible to bacteria that circulate in retained urine. When the bladder becomes stretched from retained urine in the bladder, the capillaries become occluded, preventing the delivery of metabolic and immune substrates to the bladder wall.
- The key to avoiding CaUTIs is avoiding high intravesical pressure and overdistention of the bladder, thus preserving an adequate blood supply to the bladder wall.
Written by: Gina B. Carithers
March 2021
© 2021 Digital Science Press, Inc. and UroToday.com


