Intermittent catheterization can have a significant physical and/or emotional impact on patients’ lives.
Patients may be concerned about the discomfort associated with intermittent catheterization(IC), the need to maintain privacy, the fear of performing the catheterization, and the inability to find a clean and appropriate toilet or bathroom for catheterization when traveling outside their home. Clinicians need to consider these patient concerns in their teaching and recommend possible strategies.
Teaching Catheterization:
Successful intermittent self-catheterization (ISC) requires education and support, particularly during initial teaching and follow up. Although long term ISC is safe and well accepted, an early dropout rate of about 20% has been described in children and adolescents (Pohl et al., 2002), so good support, professional instruction on catheterization technique and periodic follow-up is necessary to obtain and maintain patient compliance. A knowledgeable and experienced clinician, in most cases a nurse, is an important component for successful self-catheterization teaching. The nurse should assess what the patient and/or the person performing the catheterization knows about the urinary tract and functions of the bladder. Providing an overview of anatomy with pictures or the use of an anatomic model of the perineum can be very helpful. Many catheter manufacturers have visual guides or videos that can be used when teaching patients and/or caregivers.
Other teaching components include how to handle the catheter, identifying the urinary meatus, and care of the catheter. It is important that patients and/or the person performing the catheterization demonstrate understanding and/or ability or perform catheterization under the supportive supervision of the nurse.
Teaching Environment:
Most adults learn best under low to moderate stress, so it is important to teach self-catheterization in a low stress setting. The nurse should also assess the patient’s ability to learn intermittent self-catheterization (ISC), motivation to continue long-term catheterization, awareness of problems associated with catheterization, and the understanding of how to avoid possible complications. Other factors to consider are the patient’s bladder capacity (still voiding some amounts or complete retention), adequate bladder outlet resistance (absence of urethral scarring, strictures or enlarged prostate), absence of urethral sensitivity to pain with catheterization, and patient’s possible fear of catheterization. Initially, many patients may be extremely reluctant to perform any procedure that involves the genitals, but this is basically a “fear of the unknown.” Determining acceptance of intermittent catheterization is vital because non-compliance is seen in many patients, particularly adolescents.
General Assessment:
Many clinicians are concerned about teaching an older patient ISC but age is not necessarily a determinant to the success of ISC. Disabilities, such as poor eyesight or blindness, poor hand dexterity, lack of perineal sensation, tremor, mental disability, and paraplegia, do not necessarily preclude the ability to perform ISC. But these obstacles may be difficult to overcome in some patients and caregivers. Teaching a patient with a spinal cord injury maybe even more of a challenge because motor and sensory impairment may require changes to catheterization techniques. Impaired cognitive function can affect success in being able to carry out the procedure independently.
Important Medical History:
Any previous experience with catheterization (e.g indwelling or IC) should be determined prior to teaching a patient ISC as this will direct the teaching and should be considered when choosing a catheter. In a male patient, a history of urethral strictures or scarring or enlarged prostate may indicate need for a Coudé tip catheter. If a woman has pelvic organ prolapse, angling the catheter around the prolapse may be needed.
Choosing the catheter:
With advances in catheter technology, the number of catheter types and designs has increased, adding complexity to the catheterization process for both the nurse and the patient. Catheter types are now gender specific, long length for males, shorter length for females. acknowledging the anatomical differences in urethral length between men and women.
Design changes include the integration of all needed equipment (such as catheter, water-based
lubricant, and drainage bag) into a compact and user friendly system. These are referred to as “closed systems or kits”. But some patients with limited dexterity may find it difficult to advance a catheter through a collection bag.

When recommending a catheter, consider the patient’s lifestyle including plans for catheter storage, carrying, and disposal. Offering a selection of three to four types of catheter is recommended.
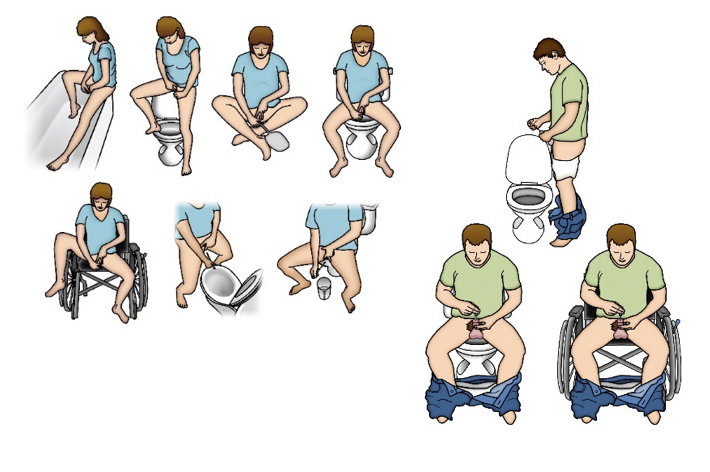
Catheterization Position:
IC teaching includes identifying the best position for performing catheterization and it should be individualized for each patient. Variables to consider when assessing a patient for the ideal position includes abnormally high body mass index and body hiatus (large pannus) as both could restrict perineal and urethral access. Most patients tend to catheterize in their bathroom, sitting on or standing in front of a toilet. For someone who is in a wheelchair most of the day, catheterizing while sitting in the chair is an option but maybe more difficult for women. Women may choose to use a mirror to visualize the urethra is also an option.
Catheterization Schedule:
The frequency of catheterization depends on patient history and the clinical reasons for initiating an IC program: for example, the individual with reflux and symptomatic UTI will require more frequent catheterizations than the person who is using IC to manage leakage caused by incomplete emptying and who has no UTI symptoms. A catheterization schedule can be recommended based on frequency-volume records, functional bladder capacity based on urodynamics findings, ultrasound bladder scans for PVR, and the impact of catheterization on a patient’s quality of life. As a general rule, bladder volume should not exceed 500 mLs, and some advocate not exceeding 400 mLs. Based on an individual’s average output, catheterization is usually performed four to six times during the day. Many patients, especially older patients, may need to catheterize at bedtime and during the night. The bladder should be emptied completely with each catheterization. When starting intermittent catheterization, the patient and/or caregiver should record the amount of urine drained from the bladder. If the patient voids, catheterization should always be performed after voiding.
Catheter Use and Care:
As there are no clear guidelines about the length of time for catheter use if the patient is re-using an uncoated catheter, re-using the same catheter for multiple catheterizations is not

recommended. The cleaning of the catheter between uses has no basis in research because there are no published randomized controlled clinical trials of cleaning methods. The comparative effectiveness of cleaning methods, therefore, is unknown.
Currently, catheter manufacturers do not provide instructions for catheter re-use or cleaning. So best practices do not support the re-use of single-use catheters at this time.
There are no set guidelines for monitoring patients performing ISC, although many urologists advocate regular urine cytology and cystoscopy with random or targeted bladder biopsies.
In reality, many patients performing intermittent catheterization are lost to urologic follow up.
March 2021
© 2021 Digital Science Press, Inc. and UroToday.com