Treatment options:
1. Nephrectomy/Adrenalectomy
2. Systemic Therapy
This patient actually underwent systemic therapy. Symptoms resolved. He is now 4 months into treatment and feeling well.
Presenter 1: Rodney Breau, MD, University of Ottawa, Ottawa, ON
Rodney Breau, MD started off by arguing against CNx in this patient. He came right off the bat by citing the CARMENA study (ASCO 2018, Mejean et al.; now published NEJM). In this study, patients were randomized to either CNx or systemic therapy (sunitinib). Sunitinib alone was not inferior to CNx + sunitinib (median OS 18.4 vs. 13.9 months, HR 0.89, favoring sunitinib). He didn’t get into some of the limitations, which Flanigan highlighted later.
He then went back to the beginning, which was Flanigan’s original seminal paper demonstrating the survival benefit of CNx in the interferon area. However, he notes that there is a subset of 30% of patients that died within the first 6 months in both arms – which indicates that there is a population of patients that have aggressive disease and will do poorly. This is present in all subsequent studies. This population perhaps would not be well suited for upfront surgery – with its associated delay to systemic therapy and QOL impact.
- CNx is not without its harms
- 30% of patients who undergo CNx never make it to systemic therapy
- So, if we are going to expose patients to the greater harms of CNx then there must be some evidence of reasonable long-term survival benefit
He again cited the CARMENA study (ASCO 2018, Mejean et al.; now published NEJM). Sunitinib alone was not inferior to CNx + sunitinib (median OS 18.4 vs. 13.9 months, HR 0.89, favoring sunitinib).
- 2% perioperative death with CNx
- 39% perioperative complications with CNx
- 18% never got systemic therapy (compared to only 5% in the sunitinib arm)
Based on this, the standard should be systemic therapy. However, he accepts that upfront CNx should be offered to patients who:
1. Need palliation of local symptoms (through chemo and radiation may achieve this too)
2. If the plan is for complete metastasectomy (low enough volume disease that systemic therapy isn’t planned)
3. When the metastases are small enough that they may be observed
Presenter 2: Robert Flanigan, MD Loyola University, Chicago, IL, USA
Robert Flanigan, MD, a recognized expert in the field, who has had an interest in the role of CNx for his entire career, weighed in on the opposite end. However, it was a balanced response.
He first started by highlighting the MSKCC risk stratification used in CARMENA. By definition, 57% of the patients were intermediate risk and 43% were poor risk – associated with a 14 and 5-month median survival, respectively.
In his own original SWOG paper (Flanigan NEJM 2001), while CNx was associated with a survival benefit, it was much more pronounced in the Performance Status (PS) 0 patients than in the PS 1 patients (6 months vs. 2-month survival benefit, respectively). Interestingly, most of the CARMENA patients would fit in the latter category – so not as much benefit would be expected in that trial. His original study also found that patients with lung-only metastases did better with CNx.
Theoretical advantages of upfront CNx:
1. palliative/reduce complications related to primary tumor
2. Remove potential sources of new metastases and new mutations
3. Improve immune function
4. Treat within a window of respectability
5. Best response (CR) to systemic therapy alone is relatively low
6. The primary tumor is often minimally responsive to TT (targeted therapy)
7. 90% of patients in TT trials had CNx
Theoretical advantages of initial systemic therapy:
1. Palliation of symptoms of metastases
2. Stabilize/regression of the disease
3. Shrinkage of tumor (albeit modest) – rarely affects surgery
4. “Litmus test” - ~30% of patients won’t make it to CNx due to disease progression, and probably wouldn’t have done well with a surgery anyway.
Retrospective series and meta-analyses have continued to demonstrate a survival benefit to CNx in the setting of mRCC in the targeted therapy era. (Heng et al. EU 2014, Bhindi et al. J Urol 2018) However, this has primarily been in IMDC favorable or intermediate risk patients (IMDC 1-3 risk factors). Dr. Rendon’s recent unpublished work presented earlier in the meeting, a meta-analysis of all CNx trials/studies in the TT era, looked at 18,570 patients – and found that CNx benefited patients (HR 0.57 favoring CNx).
Flanigan noted that only 35% of patients in the TT era are even receiving a CNx currently – so this has to be a multi-disciplinary approach to patient selection!
He also discussed the CARMENA study. Patients with low-volume metastatic disease (low-intermediate risk) were actively excluded by the investigators due to low equipoise – leaving a population that was heavily high-intermediate (60%) or poor risk (40%). They also only recruited 450 of the expected 576 patients. Sunitinib alone was not inferior to CNx + sunitinib (median OS 18.4 vs. 13.9 months, HR 0.89, favoring sunitinib). However, most of the benefit appeared to come from switching from progressive disease to stabilizing disease – no net improvement in CR or partial responses. Mortality for nephrectomy was minimal (4 deaths, 2%). Most complications were Clavian-Dindo Grade 1-2. 16% were Grade 3-4. Secondary nephrectomy in the sunitinib arm was completed in 38 patients (17%) - 7 (18.9%) were due to symptoms and considered emergent. Importantly, 22.5% of patients never recovered enough after CNx to receive sunitinib.
- He noted that in the CNx arm, 7% never got CNx and 18% never got sunitinib; in the sunitinib arm, 5% never got sunitinib, but 17% did receive a nephrectomy – so this may skew the data
- In a novel analysis that is still preliminary, when removing the patients who did not receive the therapy they were supposed to and shuffling patients based on actual treatment, there is a 17% shift in survival – now favoring CNx!
He cited Dr. Motzer and Dr. Russo’s NEJM editorial, which he agreed with:
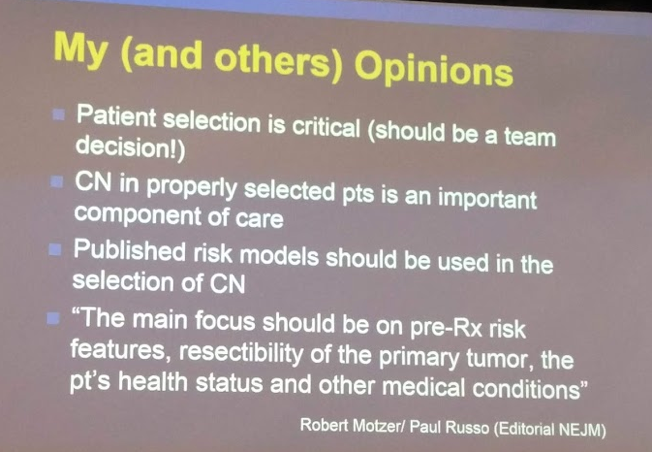
As such, as the study is flawed, CNx is not out of the question – in fact, with the appropriate patient selection, is should still be utilized. CR is best achieved in mRCC with a multi-disciplinary approach, including CNx, metastasectomy and systemic therapy.
Presented by:
Rodney Breau, MD, University of Ottawa, Ottawa, ON
Robert Flanigan, MD, Loyola University, Chicago, IL, USA
Written By: Thenappan Chandrasekar, MD, Clinical Fellow, University of Toronto Twitter: @tchandra_uromd at the 73rd Canadian Urological Association Annual Meeting - June 23 - 26, 2018 - Halifax, Nova Scotia


