Since 2013, the authors’ institution has been complying with the enhanced recovery after surgery preoperative clinical pathway recommendations (ERAS). As a result, they modified their institutional traditional preoperative cystectomy pathway, abandoning bowel preparation and changing the antibiotics regimen (supplanting intravenous ampicillin, gentamycin and metronidazole for a single dose of intravenous ceftriaxone). The aim of this study was to analyze the SSI rate within the last decade and try to elucidate the associated risk factors.
Using their institutional retrospective database of radical cystectomy patients, 287 patients undergoing RC between 2004 and 2014 were assessed. Patients’ medical records were reviewed for SSI as defined by the CDC guidelines published in 1999, namely, wound infection within the first postoperative month associated with either a) purulent discharge (with or without a positive wound culture), or b) pain, local erythema and swelling requiring wound drainage. Uunivariate and multivariate analyses were performed to determine putative predictors of SSI.
Of the 287 patients, 62 (22%) were diagnosed and treated with SSI, 43 (69%) of whom had a positive wound culture. In only 14 patients (32%) the isolated pathogen was sensitive to the administered perioperative antibiotic. Statistically significant differences were found between patients with SSI compared to those without. SSI patients had higher mean BMI, age adjusted Charlson score, undergoing surgery more recently, higher percentage of ileal conduit diversion and more patients being hospitalized in the Intensive care unit (ICU). Multivariable analysis demonstrated that increased mean BMI, ileal conduit diversion (compared to orthotopic), and contemporary surgery during recent years, were associated with increased SSI risk.
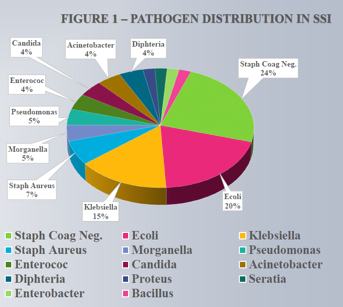
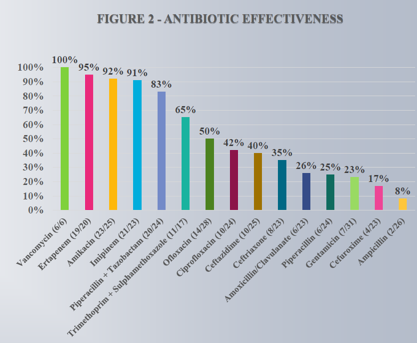
The most common pathogens were Coagulase-negative staphylococci, Ecoli and Klebsiella (Figure 1). With the exception of Vancomycin, Ertapenem, Amikacin, Imipinem and Piperacillin + Tazobactam, all other antibiotics were significantly less effective, due to high resistance rates in SSI causing bacteria (Figure 2).
In summary, a fifth of the patients undergoing RC developed SSI, especially in recent years, after ERAS implementation. As ERAS has been shown to lower SSI rates, these findings probably reflect the increasing number of morbid and more complex patients undergoing RC in recent years.
Speaker: Hanan Goldberg, Toronto, Canada
Written By: Hanan Goldberg, MD, Urologic Oncology Fellow (SUO), University of Toronto, Princess Margaret Cancer Centre
at the 2017 AUA Annual Meeting - May 12 - 16, 2017 – Boston, Massachusetts, USA


