EVALUATION
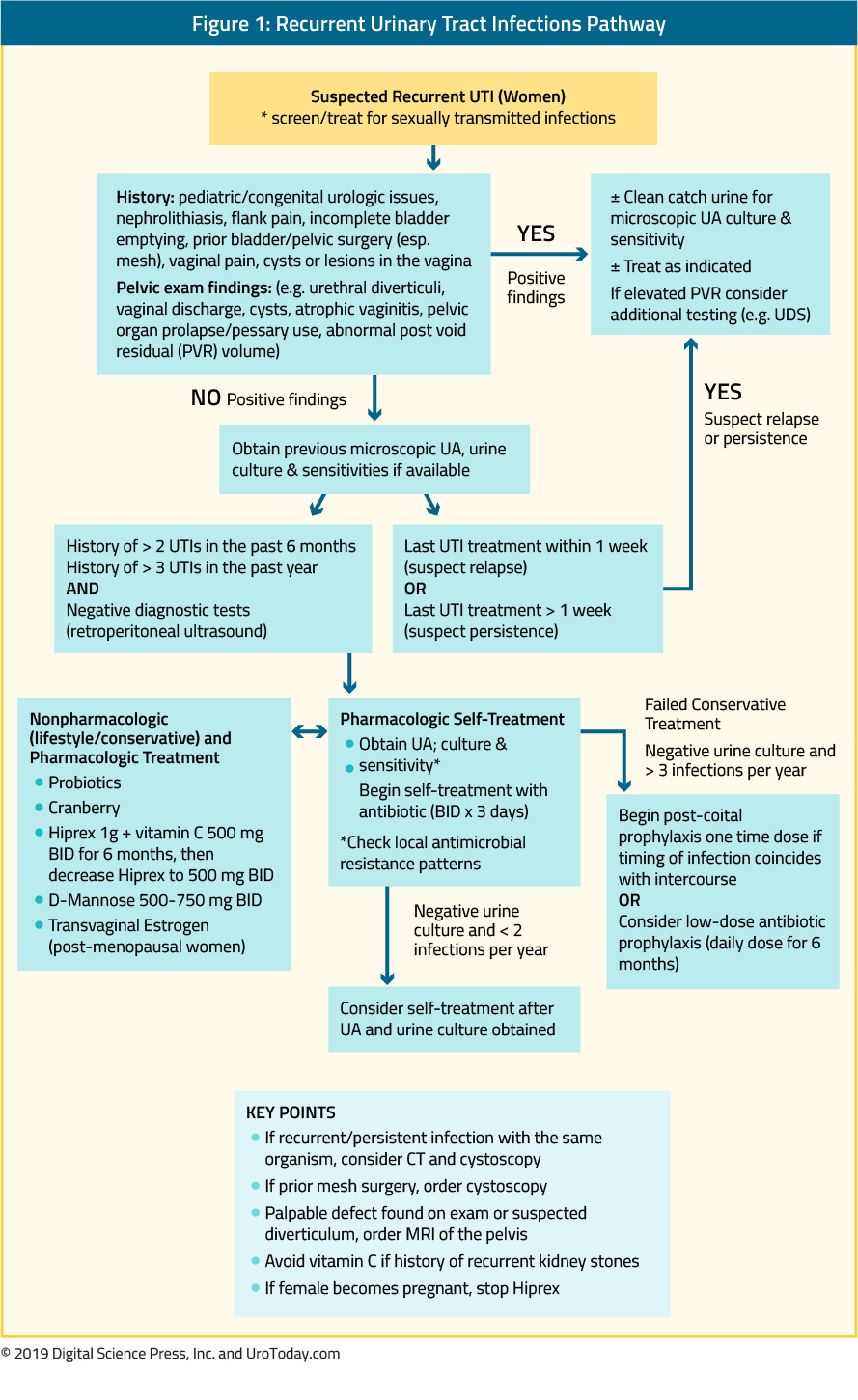
Recurrent Urinary Tract Infections (rUTI) is defined as: >2 culture-positive UTIs in 6 months or >3 in one year
1. Take A History - Document symptoms and signs that characterize rUTI episodes and exclude other disorders that could cause the patient’s symptoms (e.g. bacterial vaginosis, vaginal yeast infection, STIs). Ask about the relationship of UTIs to sexual activity, prolonged bladder holding, and bowel irregularity. Rule out noninfectious pelvic and urinary tract sources of symptoms (e.g. overactive bladder, radiation cystitis, bladder pain syndrome, vulvodynia, pelvic organ prolapse, urinary retention/poor bladder emptying, and neurogenic bladder).
Genito-urinary history: Evaluate for complicating factors including pediatric/congenital urologic conditions (e.g., vesicoureteral reflux, megaureter), nephrolithiasis, flank pain, incomplete bladder emptying, prior bladder/pelvic surgery (especially use of mesh material), vaginal pain, cysts or lesions in the vagina, antiestrogen use, pelvic malignancy, absorbent pad use, fecal incontinence, immunosuppression, and neurologic disease.
Review prior urine culture results to confirm rUTI diagnosis with two or more positive cultures in 6 months or 3 or more in one year.
2. Perform Physical Exam to include a pelvic examination - Assess for hygiene and fecal contamination, look for urethral diverticulum, vaginal discharge and/or yeast, vaginal cysts, atrophic vaginitis, and pelvic organ prolapse. If prior mesh or pelvic surgery, consider cystoscopy if a vaginal cyst or periurethral fluctuance (pseudo-urethral abscess formation) order pelvic MRI with coil.
3. Collect Urine Specimen for Testing - Send urine specimen for urinalysis (UA) if symptoms suggestive of UTI. If positive, send the specimen for urine culture and sensitivities. If microscopic hematuria in the absence of infection work-up alongside initial therapy. If sterile pyuria, rule out STIs and urinary TB (AFB’s). If asymptomatic bacteriuria, do not treat. Assess for bacterial persistence, if present considers cross-sectional imaging (retroperitoneal ultrasound) and +/- cystoscopy.
4. Perform ultrasound (bladder scan) US PVR (immediately after voiding) - if >150 cc (on 2 separate occasions) and monitor. Consider intermittent self-catheterization if no other source for infection identified and 1st line suppression fails.
TREATMENT
1st Line Therapy (Behavioral/Lifestyle Modifications) and UTI Prevention Measures- Diabetic patients: Control blood glucose and avoid glucosuria
- Fluid intake: Maintain adequate hydration (Hooten recommended drinking 1.5 L of water daily along with the suggestion to start a 500 mL bottle of water at the beginning of every meal and fully drink it before the next meal).
- Dietary Changes: Cranberry use in all its forms is not supported by current evidence; however, little harm is associated with its use.
- Probiotic: Use of either oral or intravaginal probiotics to restore the natural vaginal microbiota (Lactobacillus spp. colonies) seems to be a promising approach to reducing antibiotic consumption and to decreasing antimicrobial resistance. Lactobacilli may especially be useful for women with histories of recurrent, complicated UTIs or on prolonged antibiotic use. Dietary sources of probiotics may be helpful, these include probiotic yogurt (such as Activia), Greek yogurt, kefir and kombucha juice.
- Voiding habits: Avoid prolonged holding of urine, avoid delaying urination (peeing)
- Hygiene: Avoid disruption of normal vaginal flora with spermicides and/ or harsh cleansers. Avoid soaking in tubs, hot tubs and in baths.
- Sex: Void before and after intercourse and avoid sequential anal and vaginal intercourse
- Bowel Regimen – If diarrhea and/or fecal incontinence are present start loperamide. If mild-moderate constipation is present begin bowel regimen including increasing dietary fiber, stool softener, and/or Miralax. If moderate-severe constipation is present begin bowel regimen (as above) if not on one and consider referral to Primary Care/GI if refractory.
- Persisting irritative bladder symptoms: Many women experience irritative bladder symptoms of pressure or discomfort, bladder urgency, burning when peeing after adequate antibiotic treatment. These symptoms can mimic UTI symptoms and many women are erroneously prescribed another antibiotic but do not exhibit a relief of these irritative symptoms. Consider one of the following treatment regimens:
- Prescribe Urelle 81 mg tab, 4 times a day (evenly spaced). Take each dose with a full glass of water (8 ounces/240 mL). Can take with food if GI upset occurs.
- Over-the-counter medications:
- Azo-Pyridium (phenazopyridine) 100 mg or Uricalm MAX 99.5 mg (phenazopyridine). These are not prescription medications but can be found at most pharmacies or drug stores.
- NSAID (Motrin, Aleve) as the symptoms of UTIs are mostly connected to the inflammatory reaction of the urinary tract due to a significant increase in urinary prostaglandin production, because the onset and duration of clinical symptoms of UTI seem to be strongly connected to prostaglandin levels. Since NSAIDs can inhibit the biosynthesis of prostaglandins, they can be useful in alleviating the symptoms of UTI.
Follow up in 6 months with the maintenance of records of all symptomatic episodes, antibiotic use, UA, and urine culture results. If 2 or more infections in 6 months move to 2nd line therapy.
2nd Line Therapy (Medications)
Review and Reinforce 1st line Therapy +
- In Postmenopausal Women with rUTIs:
- Initiate transvaginal (topical) estrogen and lactobacillus containing probiotics daily. Vaginal estrogen can be prescribed as Estrace cream 1 gram or Premarin cream 0.5 grams, Vagifem (Yuvafem) 10 mcg tablets (all can be used daily for 2 weeks then twice weekly), Estring, or compounded estrogen for approximately $50 a tube.
- Estrace cream comes with 1 applicator that always has to be cleaned. Go on the manufacturer's website (www.estracecream.com), click “Request Applicators” and get 24 individually wrapped applicators at no cost, every 3 months.
- If already on these measures or they are contraindicated or ineffective after 6 months, add methenamine hippurate (Hiprex) 1 gram twice daily plus vitamin C 500 mg twice daily.
- Avoid Vitamin C if history of kidney stones
- If renal insufficiency/decreased GFR, dose methenamine hippurate accordingly
- In severe cases, consider combined initial therapy with vaginal estrogen, probiotics, methenamine hippurate and vitamin C.
- An alternative to methenamine hippurate is d-Mannose 500- 750 mg twice/day, a monosaccharide that can be rapidly absorbed and excreted by the urinary tract and can prevent the adhesion of type 1 bacterial fimbriae (bacterial virulence factor, usually caused by E. coli) promoting UTI to the uroepithelium
- In Premenopausal Women with rUTIs
- With Post-Coital rUTIs:
- Initiate a single low dose prophylactic antibiotic* within 2 hours of sexual activity for 6-12 months duration OR
- Has already tried post-coital antibiotics, or has intercourse more than twice per week initiate methenamine hippurate 1 gram twice daily, vitamin C 500 mg twice daily and lactobacillus containing probiotics daily or alternative to methenamine hippurate is d-Mannose 500- 750 mg twice/day.
- With Post-Coital rUTIs:
- With rUTI unrelated to sexual activity:
- Consider daily low dose prophylactic antibiotic* for 6-12 months’ duration OR
- Have already tried daily antibiotics, initiate methenamine hippurate 1 gram twice daily, vitamin C 500 mg twice daily and lactobacillus containing probiotics daily or alternative to methenamine hippurate is d-Mannose 500- 750 mg twice/day
Follow up in 6 months with the maintenance of records of all symptomatic episodes, antibiotic use, UA, and urine culture results. If refractory; consider an evaluation with cross sectional imaging +/- cystoscopy. In refractory patients, alternative prophylactic antibiotics can be tried. In severe refractory cases in patients on intermittent catheterization, intravesical gentamycin can be considered.
Published Date: September 26th, 2019


