Dating back to 1982, Dr. Donald Skinner was one of the first to suggest that patients who probably benefit the most from a meticulous dissection are those with clinically undetectable micrometastases to a few nodes. Since then, registry population-level studies suggest that the main factors affecting survival in patients undergoing cystectomy are disease stage and number of lymph nodes examined. What constitutes the ideal extent of dissection is still debatable:
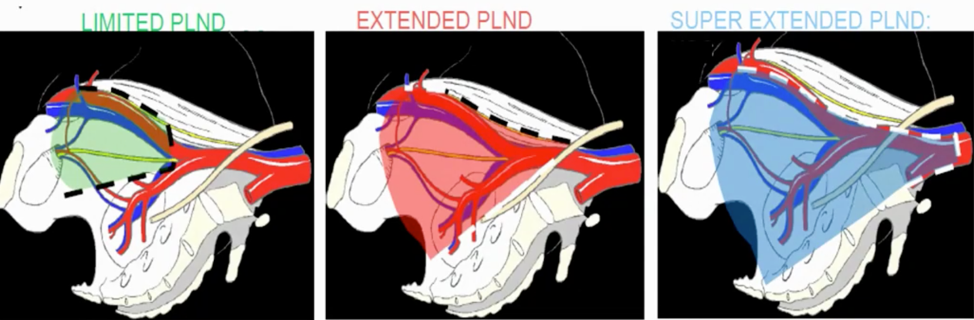
In 2010, Dr. Thalmann’s group published a mapping study of primary lymphatic landing sites among patients with bladder cancer.1 In this study of 60 patients undergoing radical cystectomy, flexible cystoscopy-guided injection of technetium nanocolloid into one of six non-tumor-bearing sites of the bladder for preoperative detection of radioactive lymph nodes with SPECT/CT was performed followed by intraoperative verification with a gamma probe. They found that a median of 4 (range: 1-14) radioactive lymph nodes were detected per site and patient, including 92% of all lymph nodes being found distal and caudal to where the ureter crosses the common iliac arteries. Eight percent were found proximal to the uretero-iliac crossing, none without simultaneous detection of additional radioactive lymph nodes within the endopelvic region. Importantly, extended pelvic lymph node dissection resected 92% of all primary lymphatic landing sites, whereas limited pelvic lymph node dissection resected only 52%.
In a study looking at two consecutive series of patients treated with radical cystectomy and limited pelvic lymph node dissection (n=336; Cleveland Clinic) and extended pelvic lymph node dissection (n=322; University of Bern), Dr. Thalmann notes that the overall lymph node-positive rate was 13% for patients with limited and 26% for those who had extended pelvic lymph node dissection.2 No patients had adjuvant chemotherapy or radiotherapy. There was a 5-year recurrence-free survival of patients with lymph node-positive disease of 7% for limited and 35% for extended pelvic lymph node dissection. More specifically, the 5-year recurrence-free survival for pT2pN0 cases was 67% for limited and 77% for extended pelvic lymph node dissection, and for pT3pN0 cases was 23% for limited and 57% for extended pelvic lymph node dissection (p <0.0001).
A similar study compared the University of Bern experience (n=405, extended pelvic lymph node dissection) to the University of Southern California experience (n=554, super-extended pelvic lymph node dissection).3 Patients undergoing a super-extended pelvic lymph node dissection had a higher median number of lymph nodes removed than those undergoing an extended pelvic lymph node dissection (38 vs. 22, p <0.0001) and a higher incidence of lymph node metastasis (35% vs. 28%, p = 0.02). However, these two groups had similar 5-year recurrence-free survival for pT2pN0-2 (57% vs. 67%, p=0.55) and pT3pN0-2 (32% vs. 34%, p=0.44) disease, with an overall recurrence rate of 38% equal at the two institutions. As such, Dr. Thalmann notes that there is a tipping point whereby the extent of pelvic lymph node dissection becomes less beneficial and outcomes are likely driven by disease biology.
A systematic review assessing the impact of the extent of lymphadenectomy on oncological outcomes of patients undergoing radical cystectomy assessed 23 studies reporting on 19,793 patients was published in European Urology in 2014.4 The authors planned a meta-analysis, but this was possible because of study heterogeneity. They found a high risk of bias and confounding across most studies, as well as extreme heterogeneity in the definition of the anatomic boundaries of lymph node dissection templates. Seven of 14 studies comparing super-extended lymph node dissection with limited or standard lymph node dissection reported a beneficial outcome for super-extended lymph node dissection in at least a subset of patients. Furthermore, there was no difference in outcome reported in two studies comparing extended lymph node dissection and standard lymph node dissection.
Several clinical trials are ongoing or have been published in this disease space. The AB 25/02 - LEA trial from the Urologic Oncology working group of the German Cancer Society is a prospective, randomized multicenter study to compare an extended versus limited pelvic lymphadenectomy in bladder cancer patients, which was published in 2019.5 Among 401 patients with locally resectable T1G3 or muscle-invasive urothelial BCa (T2-T4aM0), 203 were randomized to limited pelvic lymph node dissection, and 198 to extended. The median number of dissected nodes was 19 in the limited and 31 in the extended arm. Extended lymph node dissection failed to show superiority over limited lymph node dissection with regard to recurrence-free survival (RFS) (5-yr RFS 65% vs. 59%; hazard ratio [HR] 0.84, 95% confidence interval [CI] 0.58-1.22; p=0.36), CSS (5-yr cancer-specific survival [CSS] 76% vs 65%; HR 0.70; p=0.10), and overall survival [OS] (5-yr OS 59% vs 50%; HR 0.78; p=0.12):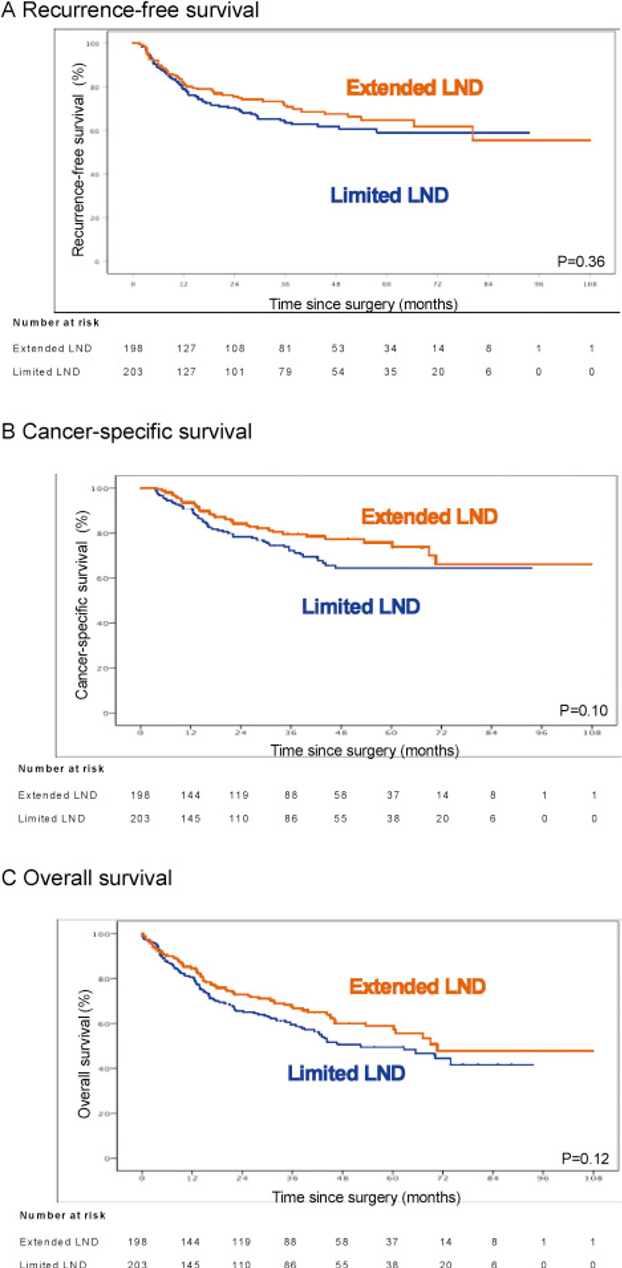
Furthermore, Clavien grade ≥3 lymphoceles were more frequently reported in the extended lymph node dissection group within 90 days after surgery. Dr. Thalmann notes that there are several possible reasons for a negative outcome in this trial, including (i) selection bias, (ii) pathological stage (% T1 disease), (iii) lack of documentation (checking the extent of resection), (iv) surgeon bias and belief.
The SWOG 1011 is still ongoing, also assessing extended versus standard lymph node dissection for patients undergoing radical cystectomy. The schema for this trial is as follows: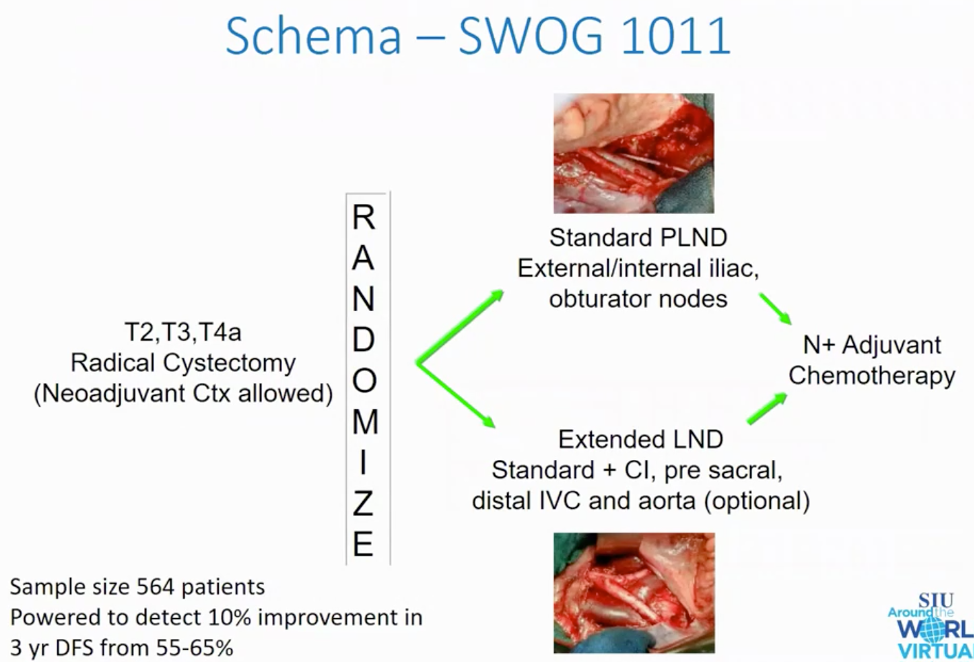
Based on the data we have (as we await further clinical trial data), Dr. Thalmann recommends an extended pelvic lymph node dissection with the following template:6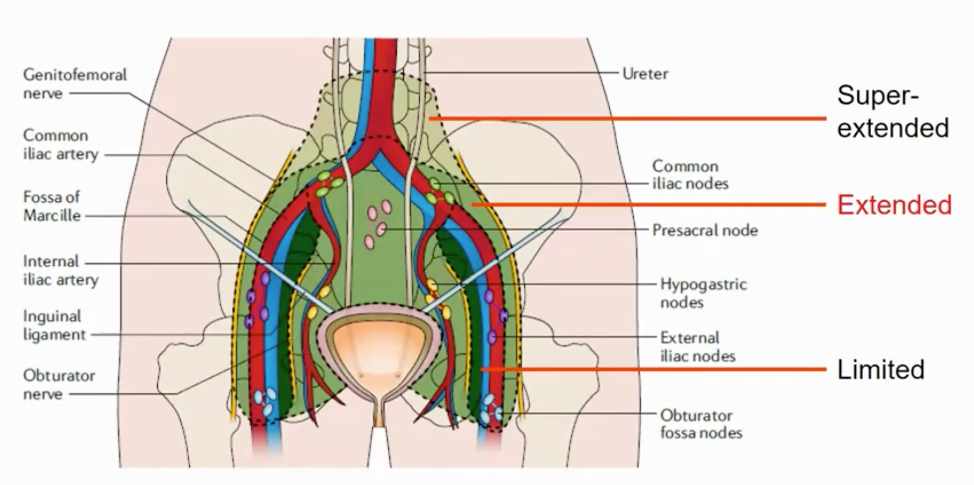
With regards to the upper urinary tract, Dr. Thalmann highlighted the 2018 Stockholm consultation on upper tract urothelial carcinoma, where several important conclusions were made:7
- There is limited evidence regarding the therapeutic advantage of lymph node dissection in upper tract urothelial carcinoma (UTUC)
- Small studies indicate significantly higher CSS for radical nephroureterectomy with lymph node dissection
- The optimal lymph node dissection template remains to be defined
- There is an increasing trend towards lymph node dissection in radical nephroureterectomy, yet this is still not consistently applied (open surgery lymph node dissection > laparoscopic surgery, lymph node yield for open > laparoscopic)
- There may be a staging benefit by providing prognostic measures valuable for CSS
- pNx disease has a worse prognosis than pN0 for T2-T4 tumors, with 5-year CSS rates of 35%, 69%, and 77% for N+, Nx, and N0 disease, respectively
Dr. Thalmann provided the following conclusions for his talk discussing lymphadenectomy for patients with urothelial carcinoma with the following take-home messages:
- Pelvic lymph node dissection is certainly better than no pelvic lymph node dissection
- Extended pelvic lymph node dissection may prove to be the standard
- Super extended pelvic lymph node dissection may not be required and may possibly be detrimental to functional outcome
- The SWOG data are eagerly awaited
- For UTUC, the data are even less solid, but a pelvic lymph node dissection is better than no pelvic lymph node dissection
Presented by: George Thalmann, MD, PhD, Department of Urology, University of Bern, Bern, Switzerland
Written by: Zachary Klaassen, MD, MSc, Assistant Professor of Urology, Georgia Cancer Center, Augusta University/Medical College of Georgia, Augusta, Georgia, Twitter: @zklaassen_md at the 2020 Société Internationale d'Urologie Virtual Congress (#SIU2020), October 10th - October 11th, 2020
References:
1. Roth, Beat, Michael P. Wissmeyer, Pascal Zehnder, Frédéric D. Birkhäuser, George N. Thalmann, Thomas M. Krause, and Urs E. Studer. "A new multimodality technique accurately maps the primary lymphatic landing sites of the bladder." European urology 57, no. 2 (2010): 205-211.
2. Dhar, Nivedita Bhatta, Eric A. Klein, Alwyn M. Reuther, George N. Thalmann, Stephan Madersbacher, and Urs E. Studer. "Outcome after radical cystectomy with limited or extended pelvic lymph node dissection." The Journal of urology 179, no. 3 (2008): 873-878.
3.Zehnder, Pascal, Urs E. Studer, Eila C. Skinner, Ryan P. Dorin, Jie Cai, Beat Roth, Gus Miranda et al. "Super extended versus extended pelvic lymph node dissection in patients undergoing radical cystectomy for bladder cancer: a comparative study." The Journal of urology 186, no. 4 (2011): 1261-1268.
4. Bruins, Harman M., Erik Veskimae, Virginia Hernandez, Mari Imamura, Molly M. Neuberger, Philip Dahm, Fiona Stewart et al. "The impact of the extent of lymphadenectomy on oncologic outcomes in patients undergoing radical cystectomy for bladder cancer: a systematic review." European urology 66, no. 6 (2014): 1065-1077.
5. Gschwend, Jürgen E., Matthias M. Heck, Jan Lehmann, Herbert Rübben, Peter Albers, Johannes M. Wolff, Detlef Frohneberg et al. "Extended versus limited lymph node dissection in bladder cancer patients undergoing radical cystectomy: survival results from a prospective, randomized trial." European urology 75, no. 4 (2019): 604-611.
6. Burkhard, Fiona C., and George N. Thalmann. "No survival benefit with extended lymphadenectomy: now what?." Nature Reviews Urology 16, no. 1 (2019): 3-4.
7. Jung, Helene, Guido Giusti, Harun Fajkovic, Thomas Herrmann, Robert Jones, Michael Straub, Joyce Baard, Palle Jörn Sloth Osther, and Marianne Brehmer. "Consultation on UTUC, Stockholm 2018: aspects of treatment." World Journal of Urology 37, no. 11 (2019): 2279-2287.


