Dr. Nappi notes that in an assessment of pooled data from 1,594 patients from 38 centers who progressed after at least 3 cycles of cisplatin-based chemotherapy and treated with either cisplatin-based conventional-dose chemotherapy or high-dose chemotherapy, there were 773 patients who received conventional-dose chemotherapy, and 821 patients who received high-dose chemotherapy.1 The 2-year progression-free survival (PFS) rate for conventional versus high-dose chemotherapy was 29% versus 50% (HR 0.44, 95% CI 0.39-0.51), and the 2-year overall survival (OS) rate was 46% versus 55% (HR 0.65,95% CI, 0.56 to 0.75) favoring high-dose chemotherapy. These results were consistent within each prognostic category except among low-risk patients, for whom similar overall survival was observed between the two chemotherapy-dose groups.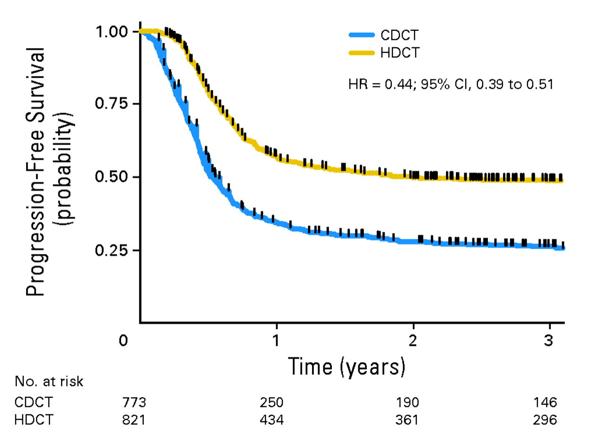

As such, Dr. Nappi highlights that salvage high-dose chemotherapy has shown better results in PFS and OS in most patients with cisplatin resistant germ cell tumor based on the most robust, albeit retrospective, evidence. There are several special patient populations that deserve mention when considering salvage high-dose chemotherapy:
- Those with brain metastasis should be treated with salvage high-dose chemotherapy and multimodal treatment should be considered for these patients
- Primary mediastinal non-seminomatous germ cell tumors carry a poor prognosis with a PFS of 25% in the Memorial Sloan Kettering Cancer Center (MSKCC) and Indian University cohorts
- Post-salvage high-dose chemotherapy residual disease should be highly considered for surgical removal given that the risk of viable germ cell tumor is ~50-70%.
In an effort to better identify patients that may (or may not) benefit from salvage high-dose chemotherapy, it is important to assess biomarker/prognostic factors. Data from the robust Indiana University experience included 364 consecutive patients who progressed after cisplatin-based combination chemotherapy and were subsequently treated with high-dose chemotherapy and peripheral-blood stem-cell transplantation.2 There were 341 patients that received two consecutive courses of high-dose chemotherapy consisting of carboplatin and etoposide, each for 3 consecutive days, and each followed by peripheral-blood stem-cell transplantation. Over a median follow-up of 3.3 years, the 2-year progression-free survival rate was 60% (95% CI, 55% to 65%) and the 2-year overall survival rate was 66% (95% CI, 60% to 70%). There were 303 patients that received high-dose chemotherapy as second-line therapy with a 2-year progression-free survival rate of 63% (95% CI, 57% to 68%), and 61 patients received high-dose chemotherapy as third-line or later therapy with a 2-year progression-free survival rate of 49% (95% CI, 36% to 61%). On multivariable analysis, poor prognostic factors identified were (i) primary mediastinal NSGCT, (ii) cisplatin refractory disease, (iii) non-seminoma histology, (iv) intermediate/poor risk The International Germ Cell Cancer Collaborative Group (IGCCCG) classification, and (v) beta-HCG >= 1,000 IU/mL prior to salvage high-dose chemotherapy.
Unfortunately, there is a long list of negative trials and no activity for immunotherapy or targeted agents in unselected patients. Dr. Nappi suggests that this may be secondary to higher tumor mutational burden in cisplatin-resistant and metastatic tissue versus cisplatin sensitive and primary gonadal disease. Additionally, p53 alterations are predominant in the cisplatin-resistant tissue and in mediastinal germ cell tumors.
As follows is a potential algorithm for assessing patients with relapse or progression after first-line chemotherapy: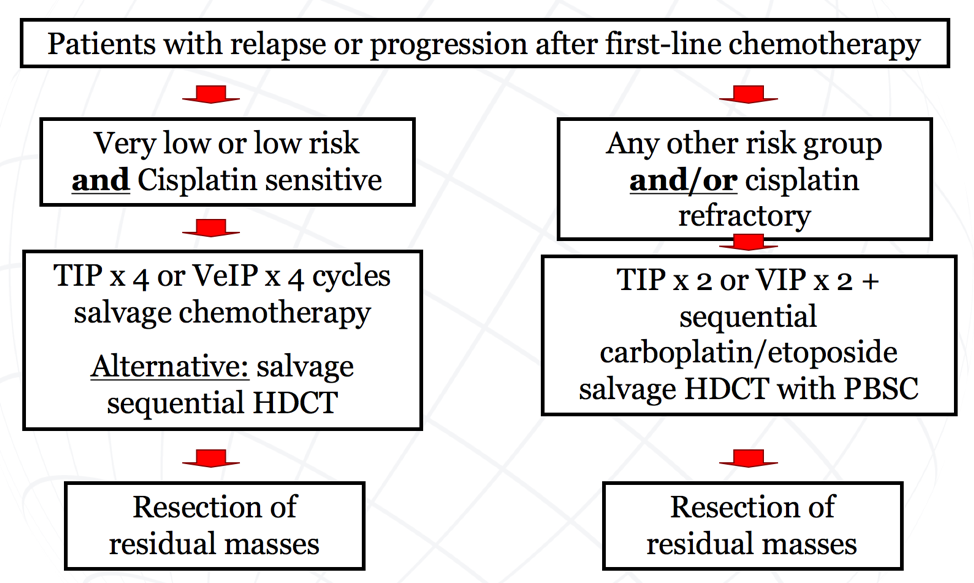
Dr. Nappi concluded her presentation with several important take-home messages regarding the treatment of refractory germ cell tumors:
- Sequential salvage high-dose chemotherapy appears to be superior to salvage conventional-dose chemotherapy and can be considered for all relapsed patients until we can safely identify those patients who are sufficiently treated with salvage conventional-dose chemotherapy
- Sequential salvage high-dose chemotherapy with carboplatin/etoposide is safe in experienced hands and appears superior to a single-high dose chemotherapy
- Salvage high-dose chemotherapy as second or later salvage therapy appears to be less effective than salvage high-dose chemotherapy as first salvage therapy
- There should be little or no debate on the use of salvage high-dose chemotherapy for a patient with poor prognosis features (ie. cisplatin-refractory disease)
- The role of salvage high-dose chemotherapy in primary mediastinal nonseminomas and in late relapses remains controversial
- Surgery remains a critical part of any salvage strategy
- Due to the complexity of relapsed germ cell tumor and the need for experienced multi-disciplinary teams, patients should be treated at high-volume, experienced centers
- There is an unmet need for biomarkers for appropriate patient selection
- Patients should be included in prospective clinical trials whenever possible, most notably the TIGER trial, a randomized trial of TIP versus TI-CE as initial salvage chemotherapy for patients with germ cell tumors
Presented by: Lucia Nappi, Assistant Professor, Urologic Sciences Dpt, University of British Columbia, Medical Oncologist BC Cancer, Senior Research Scientist Vancouver Prostate Centre
Written by: Zachary Klaassen, MD, MSc, Assistant Professor of Urology, Georgia Cancer Center, Augusta University/Medical College of Georgia, Augusta, Georgia, Twitter: @zklaassen_md during the 1st Global Society of Rare Genitourinary Tumors Virtual Summit, December 11-12, 2020
References:
1. Lorch A, Bascoul-Mollevi C, Kramar A, et al. Conventional-dose versus high-dose chemotherapy as first salvage treatment in male patients with metastatic germ cell tumors: Evidence from a large international database. J Clin Oncol2011 Jun 1;29(16):2178-2184.
2. Adra N, Abonour R, Althouse SK, et al. High-dose chemotherapy and autologous peripheral-blood stem-cell transplantation for relapsed metastatic germ cell tumors: The Indiana University Experience. J Clin Oncol2017 Apr 1;35(10):1096-1102.
Related Content:
Keynote Lecture: GSRGT 2020: Management of Chemotherapy-Resistant Germ Cell Tumors in 2020


