(UroToday.com) The 2022 EAU Section of Oncological Urology (ESOU) Annual Meeting included a session on the early detection and personalized management of testis cancer and a presentation by Dr. Asif Muneer discussing the management of indeterminate testicular masses. Dr. Muneer notes that the traditional dogma of testicular mass management is “when in doubt, take it out” (John P. Donohue, 1980), however less aggressive management options have emerged since then to safely spare testis in the right circumstances.
There are several indications for testis sparing surgery, including (i) a solitary testicle, (ii) synchronous bilateral tumors, (iii) metachronous tumors in the contralateral testicle, and (iv) indeterminate/benign lesions. Additionally, there are several advantages of partial orchidectomy:
- Preservation of Leydig cells and seminiferous tubules
- Endogenous testosterone versus testosterone replacement therapy
- Fertility preservation if there is an absent/atrophic contralateral testicle
- Removal of benign/indeterminate lesions
- Psychological impact of orchidectomy
Indeterminate testicular lesions are impalpable/incidental, have mixed echogenicity, are associated with normal tumor marker levels, and range in size from <0.5 cm to <2 cm. The majority of small testis masses are benign and thus radical orchidectomy is associated with overtreatment. However, differentiating benign versus malignant masses may be challenging.
With regards to small volume germ cell tumors, these are clearly stage I disease and associated with an excellent prognosis with radical orchidectomy. However, there may also be an option allowing for the surveillance of these small masses with interval scans and self-examinations. Recently, there has been increased detection of small testicular masses secondary to better ultrasound resolution and more imaging for benign scrotal conditions, including infertility, trauma, and pain. As such, there are several questions that arise with regards to how we should manage indeterminate lesions:
- When should we perform radical orchidectomy? Acknowledging the fertility, hormone, and body image issues
- Radiological surveillance – how and when?
- Testis sparing surgery – which lesions need excising?
In a study of 28 patients with small testis masses, Galosi et al.1 found that the mean age was 38 years old, mean lesion size was 9.3 mm, and 17 (60.7%) patients underwent testis sparing surgery. Among these patients, only 6 (21.4%) had a malignant tumor on final diagnosis. Other studies of similar sample size have found comparable results with regards to malignancy rates. When assessing these masses by ultrasonography, it is important to assess that size, echogenicity, vascularity, and TML of the mass. Risk factors for malignancy include a history of a contralateral tumor and history of cryptorchidism.
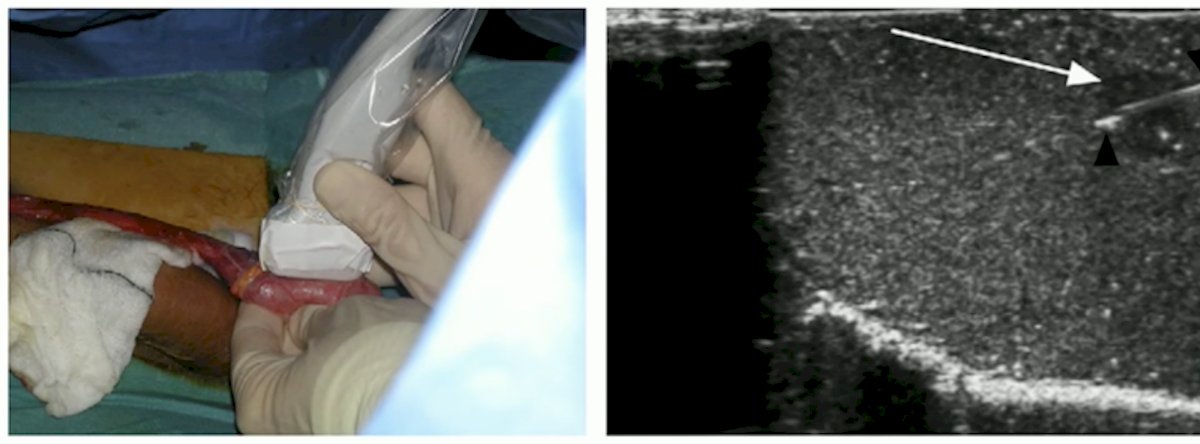
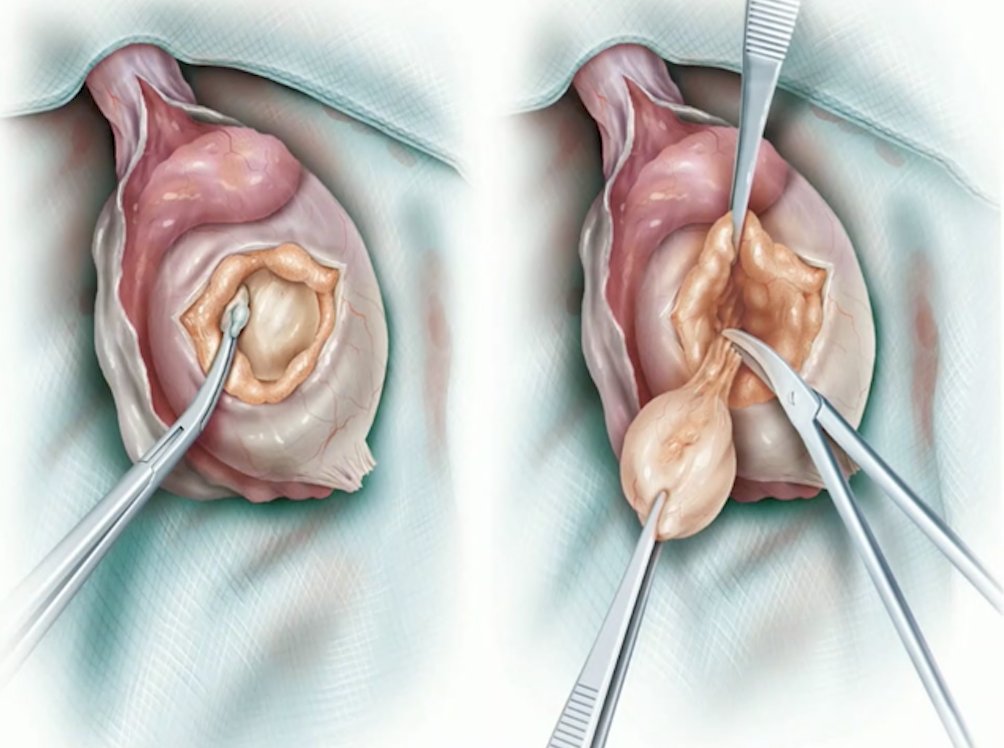
When planning a targeted excision, it is important to consider pre-operative staging, tumor markers, testosterone level, and sperm banking. Dr. Muneer performs these operations through an inguinal approach, delivering the testicle into the operative field, and preserving the gubernaculum. Subsequently, he utilizes ultrasound guidance for needle localization of the mass, equatorial incision over the targeted area, and excision of the testicular lesion.
For fertility preservation, sperm banking should be done pre-operatively, given that semen parameters can be impaired even with a normal contralateral testicle. If it is a solitary testicle, or there are bilateral tumors, one should consider testis preserving surgery or combine the procedure with oncoTESE.
Looking specifically at work from his institution (the UCL Male Genital Cancer Centre), Dr. Muneer notes that among 300 small testicular masses (<2 cm lesions), 20% had had a radical orchidectomy, with 85% (53/62) of these patients having a germ cell tumor. Appropriate patients were offered surveillance or ultrasound-guided testis cancer surgery. As follows is the malignancy rate stratified by lesion size:
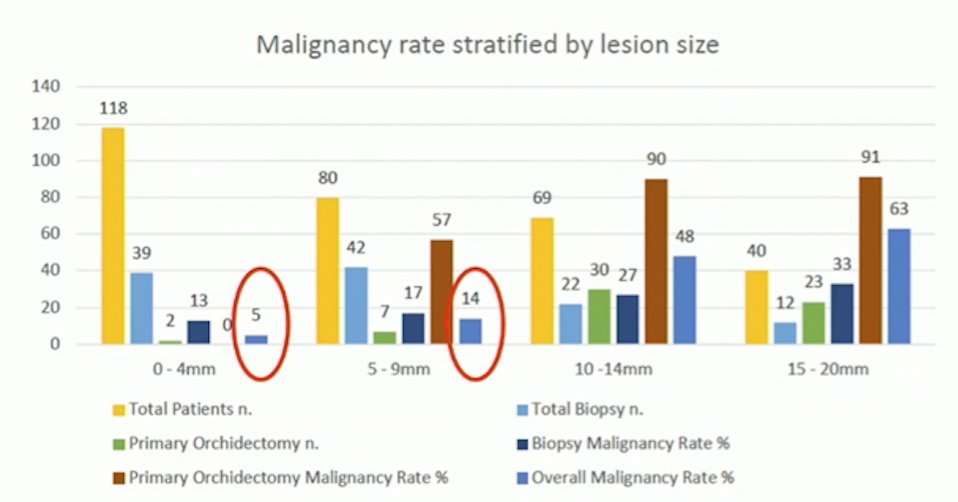
In their current series, those that had testis sparing surgery and were found to have a malignant small testis mass were managed with a completion orchidectomy and prosthesis 4-6 weeks later. Of note, among the malignant tumors, 92% had residual disease or GCNIS on completion orchidectomy pathology.
Dr. Muneer concluded his presentation of the management of indeterminate testicular masses with the following take-home messages:
- Indeterminate lesions do not require immediate orchidectomy
- Fertility preservation and endocrine function are important to the patient
- There is increased malignancy risk with larger lesions
Presented by: Asif Muneer, Consultant Urological Surgeon and Andrologist, UCL Division of Surgery and Interventional Science, London, UK
Written by: Zachary Klaassen, MD, MSc – Urologic Oncologist, Assistant Professor of Urology, Georgia Cancer Center, Augusta University/Medical College of Georgia, @zklaassen_md on Twitter during the 2022 EAU Section of Oncological Urology (ESOU) Hybrid Annual Meeting, Madrid, Spain, Fri, Jan 21 – Sun, Jan 23, 2022.
References:
- Galosi AB, Fulvi P, Fabiani A, et al. Testicular sparing surgery in small testis masses: A multi-institutional experience. Arch Ital Urol Androl. 2016 Dec 30;88(4):320-324.


