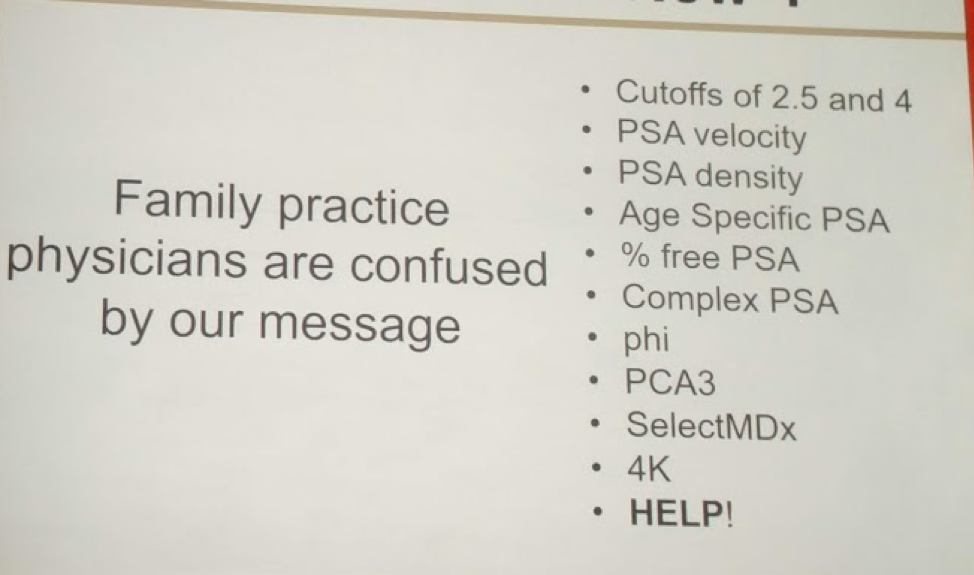
Unfortunately, beyond the changing USPSTF recommendations, there are so many biomarkers and tests that family physicians, who do most of the initial PCa screening, are confused by the message! The PSA cutoffs have changed from 4 to 2.5. Additional PSA tools, including velocity and density, were introduced. But what are they do with all of these?
In order to make it usable, we need to simplify the message for the people that actually order PSA – family physicians and internal medicine physicians. He then cited a few studies to help address his point.
In an update and review of the PLCO trial, a prostate cancer screening study flawed by contamination in the non-screening arm, they found that patients who had an initial PSA < 1.0 ng/mL had a very low rate of developing PCa in the following 5 years. So, this was the first evidence that low PSA could help reduce PSA screening.
Crawford’s team explored this further.1 They used the 350,000 Henry Ford HMO system to determine what initial PSA values could tell us about future PCa risk. Median PSA was 1.0, mean age 55, 30% African-American. In this important study, they found that patients with PSA < 1.5 had a 0.51% risk of developing prostate cancer. Yet, with a PSA between 1.5-4.0, the risk increased 15-fold to 7.85%, and in PSA > 4.0, risk was 10.39%. So, they felt that PSA 1.5-4.0 was a danger zone and needed closer follow-up. Approximately 25% of men have a PSA 1.5+; 75% of men have a PSA < 1.5.
However, he made it clear that this does not mean everyone with PSA > 1.5 gets a biopsy! It just means they need to be evaluated for PCa risk – with adjunct tests and biomarkers, to rule out BPH, prostatitis, etc.
Now, how do we know we aren’t missing significant prostate cancer in men with PSA < 1.5. A recent study by colleagues at the University of Toronto2, which was also presented as an abstract at AUA, demonstrated the results of an aggressive prostate biopsy in younger men (age < 50). In these men, 1.5 remained an important cutoff. With a PSA < 1, 92.9% had no cancer. In men with PSA < 1.5, 73.7% had no cancer; and only 8% had a clinically significant prostate cancer.
Lastly, he reviewed common molecular markers (4K, PHI, SelectMDx) and found that in men with PSA < 1.5, they were rarely positive, corroborating the need to be less concerned in these men.
As such, at this time, his recommend algorithm for the future is as follows:
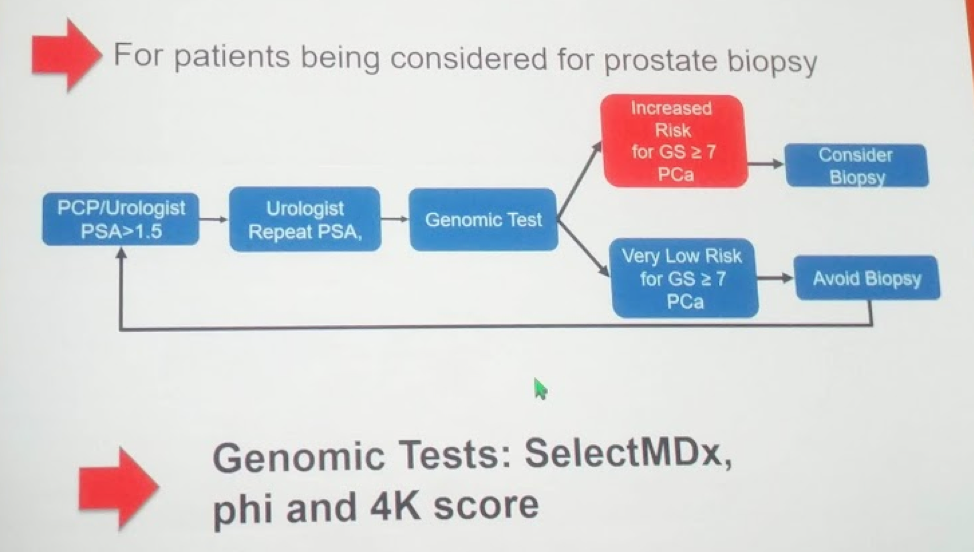
Men with PSA < 1.5 should not get a repeat PSA for at least 5 years.
Therefore, PSA 1.5 should be the new cutoff for family practitioners to remember – simple and useful. However, while this will generate a referral to the urologist, it should not automatically trigger a biopsy. Clinical tests and biomarkers should help select patients for further evaluation!
References:
1. Crawford ED, Moul JW, Rove KO, Pettaway CA, Lamerato LE, Hughes A. Prostate-specific antigen 1.5-4.0 ng/mL: a diagnostic challenge and danger zone. BJU Int. 2011 Dec;108(11):1743-9. doi: 10.1111/j.1464-410X.2011.10224.x. Epub 2011 Jun 28.
2. Goldberg H, Klaassen Z, Chandrasekar T, Wallis CJD, Toi A, Sayyid R, Bhindi B, Nesbitt M, Evans A, van der Kwast T, Sweet J, Perlis N, Hamilton RJ, Kulkarni GS, Finelli A, Zlotta A, Fleshner N. Evaluation of an Aggressive Prostate Biopsy Strategy in Men Younger than 50 years of Age. J Urol. 2018 May 11. pii: S0022-5347(18)43127-8. doi: 10.1016/j.juro.2018.05.017. [Epub ahead of print]
Presented by: E. David Crawford, MD, University of Colorado
Written by: Thenappan Chandrasekar, MD, Clinical Fellow, University of Toronto, @tchandra_uromd at the 2018 AUA Annual Meeting - May 18 - 21, 2018 – San Francisco, CA USA


