fPSA ratio cut points range from 15%-25% with higher values correlated with lower PC risk, within the PSA range of 4-10 ng/mL. However, the role of fPSA/total PSA ratio in biochemical recurrence (BCR) is unknown. The authors aimed to assess the role of fpsa/total PSA ratio in patients with BCR after radical prostatectomy.
A local institutional PC database was queried for all patients in the last decade who had BCR after radical prostatectomy and had at least one fPSA ratio blood test (after BCR). fPSA was tested either by accident, or reflexively (if PSA was at the range of 4-10 ng/ml) Patients were stratified according to their first fPSA ratio after BCR, using a cut-off of 0.15.
Cox regression multivariable analyses were performed to predict covariates associated with, metastasis castration-resistant prostate cancer (CRPC), and cancer-specific survival (CSS). A total of 305 men with BCR were found. 117 men had %Fpsa>=0.15 (group 1) and 186 patients (61.6%) had %fPSA< 0.15 (group 2).
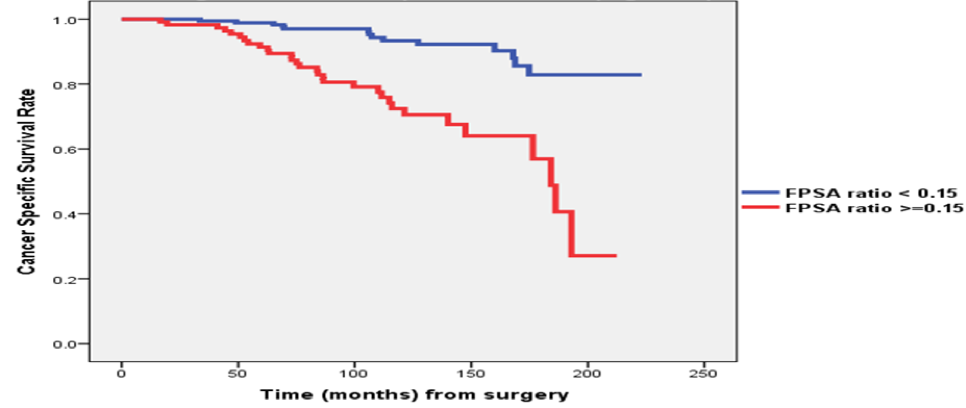
Baseline data is shown in figure 1, demonstrating similar attributes in both groups. figure 2 demonstrates the clinical outcomes of both groups, showing a clear advantage to patients with a %Fpsa <0.15 in terms of the need for salvage radiation, conversion to CRPC status, development of metastasis (especially bone metastasis). Figure 3 demonstrates that patients with a %Fpsa<0.15 have better outcomes in regard to the timing of starting hormonal therapy and becoming CRPC. Lastly, figure 4 demonstrates that cancer specific survival (CSS) is significantly improved in these patients as well. In Cox regression multivariable models predicting metastasis, CRPC and CSS, a %Fpsa ratio of >=0.15 was shown to significantly worsen each of these outcomes, with a hazard ratio ranging between 1.92 and 2.92.
Figure 1 – Baseline data

Figure 2 - Clinical outcomes
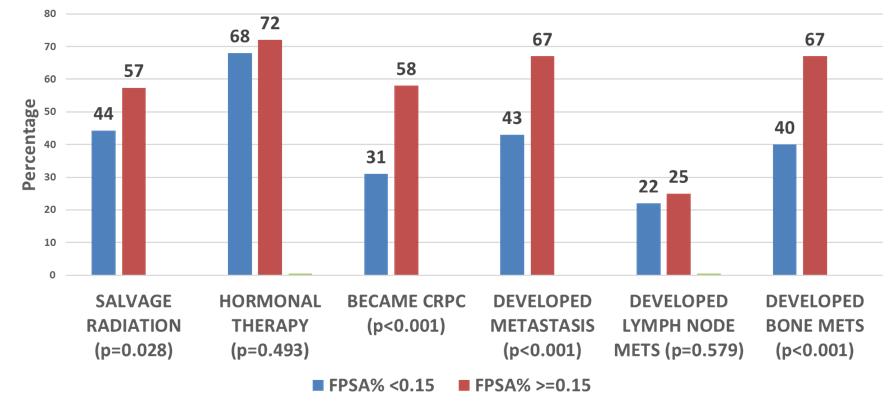
Figure 3: Timing of Clinical events
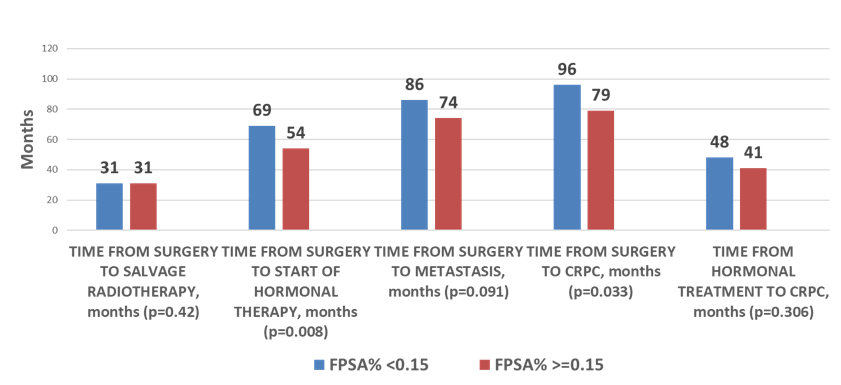
Figure 4: Cancer-specific survival
In conclusion, this study suggests that a %fPSA ratio>=0.15 in the setting of BCR after radical prostatectomy denotes a more aggressive disease, reflected in higher rates of metastasis, CRPC and cancer specific mortality. These findings suggest a reversal in the significance of fPSA ratio in the post treatment state, and a potential novel role for this widely available and low-cost biomarker.
Written by: Hanan Goldberg, MD, Urologic Oncology Fellow (SUO), University of Toronto, Princess Margaret Cancer Centre @GoldbergHanan at the 2018 AUA Annual Meeting - May 18 - 21, 2018 – San Francisco, CA USA


