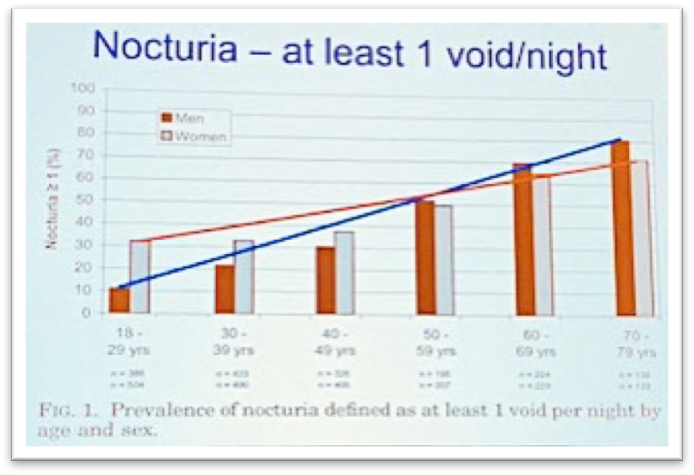
Current prevalence of nocturia was presented to introduce severity of disease occurrence by age and gender. Figure 1 shows that prevalence increases with age in both men and women.
Previous research showed that although there are known exposures associated with disease development, none of them were linked to nocturia in more than 50% of the affected men and women. Therefore, health practitioners should consider multiple risk factors when treating nocturia including patient’s lifestyle, sleep patterns, cardiovascular and neurological conditions, and other urological characteristics related to bladder and prostate health.
According to the presenters, disease leads to the multiple negative health outcomes related to sleep disturbances, metabolic disorders, overall decrease in QoL, and increase in mortality. Nocturia is known as a predictor of poor sleep quality in elderly population due to sleep deprivation. As a result, patients could develop a metabolic syndrome because sleep duration of less than 6 hours is a proxy for such condition.
Voiding diary was presented as a great tool for classification of disease etiology. Evaluation of nocturia is based on the analysis of a simple 24-hour diary of voids documented by patient. Voiding diary analysis can reveal up to 19 underlying medical conditions, which could be linked to disease emergence. However, there is a question about the most feasible type of diary used for diagnostic purposes: 24-hour FVC, complete 24h, nocturnal only, or nocturnal only plus 24h volume. Review of real-life case studies showed that correct choice depends on disease characteristics, but nocturnal only plus 24h volume diary was named to be the best option.
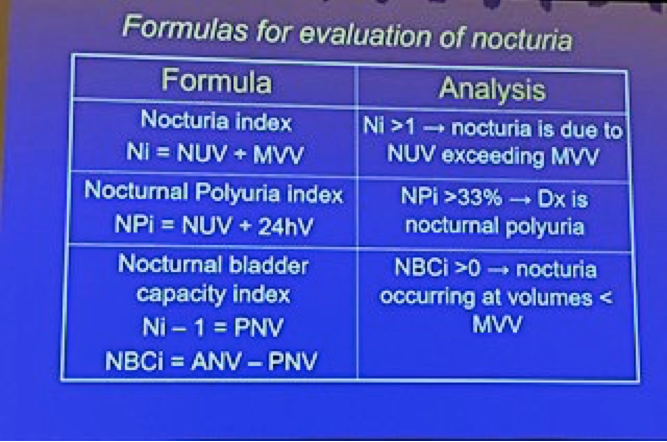
Following formulas were introduced for evaluation of nocturia (Figure 2)
Presenters introduced 4 primary types of nocturia: nocturnal polyuria (NP), diminished global/nocturnal bladder capacity (NBC), mixed, and polyuria. Possible causes of NP included sleep apnea, diuretics, SSRIs, calcium channel blockers, tetracycline, and lithium.
Instructors named intravesical obstruction, idiopathic nocturnal detrusor overactivity, neurogenic bladder, cystitis, and cancer of bladder, prostate, and urethra among causes of diminished global/nocturnal bladder capacity (NBC). Nocturnal diuresis rate (DR) was correlated with nocturia severity. DR can be beneficial in identification of individuals for whom influencing the rate of urine production may improve frequency, urgency, and nocturia.
Polyuria was linked to diabetes mellitus, diabetes insipidus, and polydipsia (primary thirst disorder).
Dr. Alan Wein has reviewed various treatment options of nocturia. He reported that in order to decrease nocturia, one has to decrease bladder activation on motor and/or sensory side, decrease nocturnal urine production, or decrease significant residual urine volume to improve nocturnal storage capacity. Dr. Wein proposed a treatment framework that considers such outcome indicators as number of nocturia episodes, time to first awakening, QoL criteria, and long-term decrease in adverse events. For the most successful treatment, it is important to first consider usual suspects: poorly controlled systemic disease, medications which are known to cause nocturia, and sleep apnea. Next, behavioral and lifestyle modifications should be introduced. Finally, there are pharmacological treatment options for other urological conditions such as overactive bladder (OAB), which might decrease nocturia episodes, but only if patient has already been diagnosed with OAB. Dr. Wein suggested that it is important to treat the most bothersome symptoms, but behavioral modifications are crucial.
Multiple studies on antidiuretics were presented during the course. Desmopressin melt (tablet) was proven to decrease nocturnal voids and improved sleep. Noctiva, desmopressin acetate nasal spray, was recommended to use in adults over 50 years of age with polyuria who awaken at least 2 times per night to void.
In conclusion, the presenter reinstated a multifactorial nature of nocturia and proposed treatment guidelines based on disease characteristics (Figure 3).

Presented by: Jeffrey P. Weiss, MD, FACS, Department of Urology, SUNY Downstate Medical Center and Alan J Wein MD, PhD(hon), FACS, is the Founders Professor and Emeritus Chief of Urology and Director of the Residency Program, University of Pennsylvania.
Written by: Hanna Stambakio, BS, Clinical Research Coordinator, Division of Urology, University of Pennsylvania, Twitter: @PennUrology at the 2018 AUA Annual Meeting - May 18 - 21, 2018 – San Francisco, CA USA
Watch Video Lectures on Nocturia;
Epidemiology of Nocturia - Interview with Alan Wein
Pathophysiology of Nocturia - Jeffrey Weiss


