This was a prospective observational study of 12 women with MS and NDO. They used a 3T fMRI to evaluate brain function during the filling phase. UDS equipment was in a separate room to minimize patient distraction. Strong urgency was signaled, and voiding was permitted. The fMRI was repeated after onabotulinumtoxinA injection, and pre and post BOLD (blood oxygen level dependent) signaling were compared.
The mean age of the patients was 44 years, and MS was stable for at least six months prior to the study. Post-void residual increased and clean intermittent catheterization was initiated in a number of patients, demonstrating a significant effect on the bladder function in the voiding phase, after onabotulinumtoxinA injection. Increased BOLD signal activation was seen in the insula, right prefrontal cortex, and cingulate cortex after treatment.
This study shows several interesting findings. First, the increased activity was seen in the cingulate and prefrontal cortices, insula, pons, and hypothalamus is different from other fMRI studies of different treatment modalities, such as sacral neuromodulation, where the BOLD activity was decreased in these areas. (Figure A and B). This is perhaps because it is a population of neurogenic bladder patients, as opposed to the idiopathic OAB patients in the other studies. Also, onabotulinumtoxinA had a strong impact in the voiding phase (demonstrated by the initiation of CIC in a large number of patients), in contrast to other therapies. Secondly, onabotulinumtoxinA increases the activity of the brain regions known to be involved in sensation and processing of urinary urgency. This demonstrates a newly proposed mechanism of action for onabotulinumtoxinA, in addition to its effects on the motor function of the bladder.

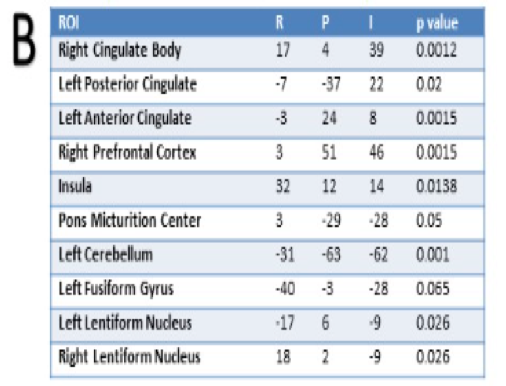 Figure 1. A shows the Regions of Interest (ROI) coordinates using MNI space and RPI coordinates system, and the p value for each ROI. B shows the subtraction BOLD activation maps of post-pre BTX-A for the ROIs. 1) Right Cingulate 2) Pons 3) Insula 4) Right Prefrontal Cortex
Figure 1. A shows the Regions of Interest (ROI) coordinates using MNI space and RPI coordinates system, and the p value for each ROI. B shows the subtraction BOLD activation maps of post-pre BTX-A for the ROIs. 1) Right Cingulate 2) Pons 3) Insula 4) Right Prefrontal CortexOverall, fMRI is a promising way to study the mechanism of OAB in both idiopathic and neurogenic patients. This very interesting study is the first to demonstrate the sensory effects of onabotulinumtoxinA injection and challenges the commonly accepted mechanism of action for this treatment modality. Future fMRI studies may elucidate new treatments for both idiopathic OAB and neurogenic detrusor overactivity.
Presented By: Rose Khavari, MD; Houston Methodist Hospital
Co-Authors: Christof Karmonik, Saba Elias, Timothy Boone
Author Affiliation: Houston Methodist Hospital, Houston, TX
Written by: Dena Moskowitz, MD; Female Pelvic Medicine and Reconstructive Surgery Fellow, Virginia Mason Medical Center; @demoskowitz at the 2018 AUA Annual Meeting - May 18 - 21, 2018 – San Francisco, CA USA
References:
- Komesu YM, Ketai LH, Mayer AR, Teshiba TM, Rogers RG. Functional Magnetic Resonance Imaging of the Brain in Women With Overactive Bladder: Brain Activation During Urinary Urgency. Female Pelvic Med Reconstr Surg. 2011;17(1):50-54. doi:10.1097/SPV.0b013e3182065507
- Weissbart SJ, Bhavsar R, Rao H, et al. Specific Changes in Brain Activity During Urgency in Women with Overactive Bladder after Successful Sacral Neuromodulation: An fMRI Study. J Urol. April 2018. doi:10.1016/j.juro.2018.03.129


