The first step in prostate cancer care is diagnosis. Typically, prostate cancer diagnosis is prompted as a result of abnormal screening results. Thus, it is particularly relevant that African American men are poorly represented in the trials of prostate-specific antigen (PSA) screening which are used to inform evidence-based prostate cancer screening guidelines. Further, the randomized trials of prostate cancer screening with PSA testing included men age 55 years and older, while many guidelines recommend screening starting at 40 years of age for higher-risk men, including African American men.
As a result, the generalizability of these guidelines to African American men is unclear, particularly among younger men. In the Prostate, Testicular, and Penile Oral Abstract Session at the 2021 American Society of Clinical Oncology 2021 Annual Meeting, Dr. Qiao presented an assessment of the association between prostate cancer screening intensity with prostate specific antigen (PSA) testing with prostate cancer outcomes in younger African American men diagnosed with prostate cancer.
To do so, the authors used data from the Veterans Health Administration to identify African American men aged 40 to 55 years who were diagnosed with prostate cancer between 2004 and 2017, based on the fact that the earliest recommended age to begin discussion of PSA screening is 40 years. The VA data utilized linked cancer registry data including tumor characteristics, pathology reports and survival data to relational databases including demographic, diagnostic, and procedural details as well as clinical notes.
Using administrative procedural codes, the authors identified PSA screening and characterized an individual’s screening intensity, defined as the proportion of years prior to prostate cancer diagnosis in which they underwent screening. The authors looked back for up to 5 years preceding prostate cancer diagnosis.
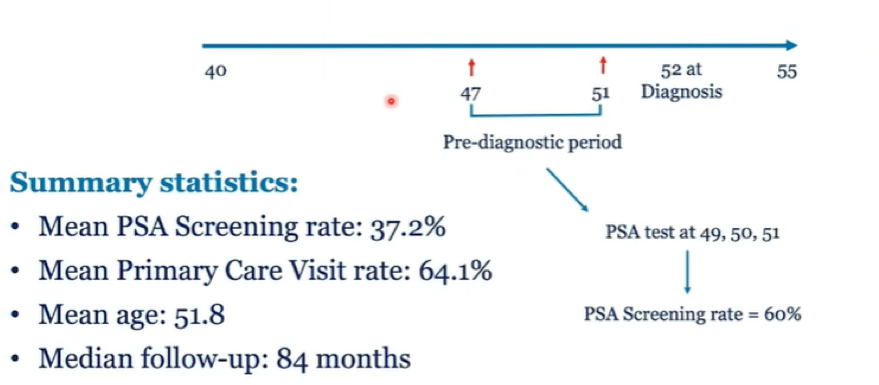
The authors then utilized multivariable logistic regression to assess the association between PSA screening intensity on metastatic disease at diagnosis. Further, they used Fine-Gray regression to examine prostate cancer specific mortality while considering non-cancer death as a competing event. In doing so, they used published screening-dependent lead times to perform lead-time correction. They further considered a dichotomized version of PSA screening intensity (High vs Low), centered on the mean.
The authors identified 4,654 African American men with a mean age of 51.8 years. Over a pre-diagnostic observation period ranged from 1 to 5 years (median = 5 years), the total screening rate was 53.2%. Overall, included patients underwent an average of 1.9 PSA tests in the 5 years prior to diagnosis. Among patients in the high PSA screening intensity group, a mean of 3.0 PSA tests were performed in the 5 years prior to diagnosis while in the low PSA screening intensity group, a mean of 0.5 tests were performed.
Patients in the high PSA screening intensity group were more likely to be older at diagnosis and have lower risk characteristics, manifest by TNM stage, histology grade (Gleason score), and PSA level at diagnosis.
Included patients were then followed for a median of 7 years.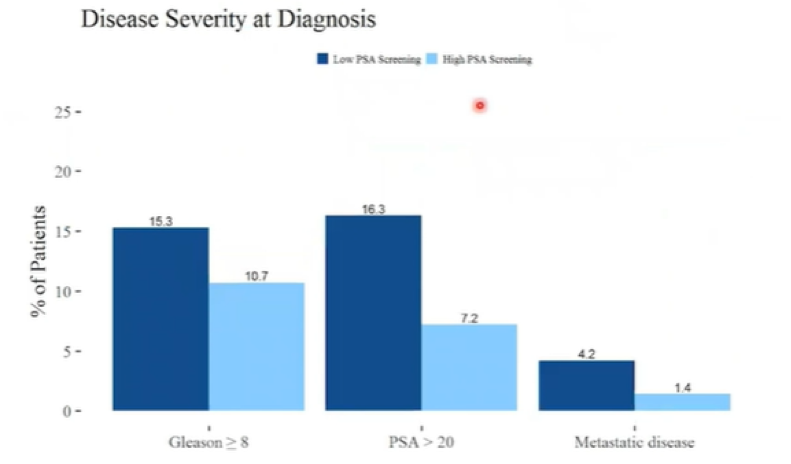
At diagnosis, patients who had a Low intensity of pre-diagnosis PSA screening had a higher prevalence of high grade histology, defined as Gleason sum ≥ 8 / Grade Group ≥ 4, (18.6% vs 14.4%, p<0.01) and of metastatic disease (3.7% vs. 1.4%, p < 0.01) than those with a higher intensity of PSA screening. Further, those with a higher intensity of PSA screening prior to diagnosis had lower cumulative incidence of prostate cancer specific mortality (2.2% vs 4.0% at 84 months and 3.1% vs 6.6% at 120 months).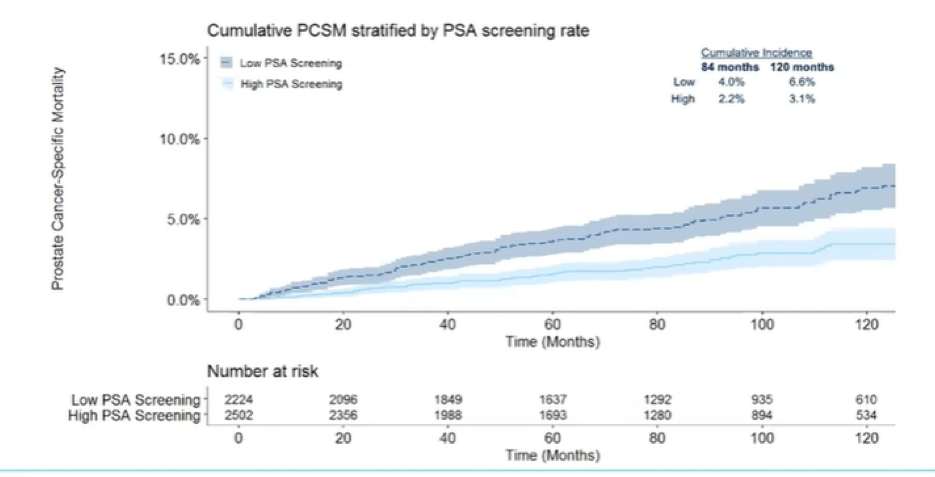
In adjusted models, increased PSA screening intensity was associated with a reduced likelihood of metastatic disease at diagnosis (odds ratio: 0.61, 95% confidence interval (CI) = [0.47-0.81], p < 0.01) and decreased risk of prostate cancer-specific mortality (sub-distribution hazard ratio: 0.75, 95% CI = [0.59-0.95], p = 0.02).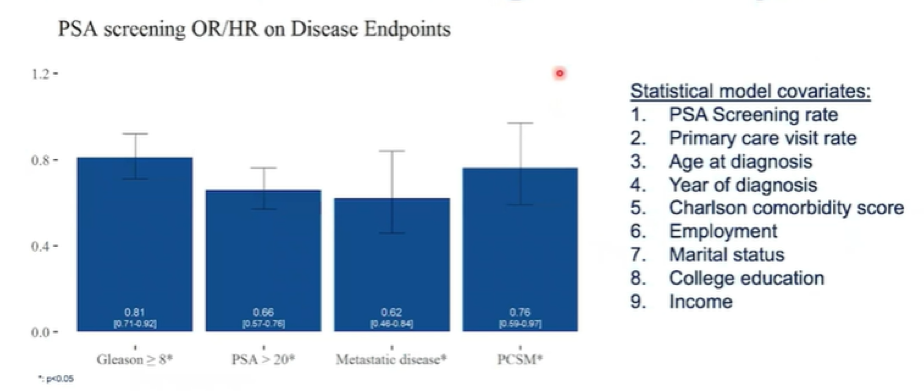
Thus, the authors concluded that this large, national cohort of younger (age 40-55 years) African American men demonstrates that increased PSA screening density prior to prostate cancer diagnosis is associated with a decreased risk of high grade histology at diagnosis, metastases at time of diagnosis and of prostate cancer-specific mortality.
Moving forward, they suggested that these data may be one step in addressing racial disparities in prostate cancer care, given that access to care barriers disproportionately affect African American men. However, to have an effect, interventions to increase access to and uptake of PSA screening among younger African American men are needed. Further, the authors point out that these data are limited as this cohort is limited to those diagnosed with prostate cancer and the lead-time correct is not validated in this group and may fail to appropriately account for the effects of this bias.
Presented by: Edmund Qiao, BS, Department of Radiation Medicine and Applied Sciences, School of Medicine, University of California San Diego, La Jolla, CA


