Thus, in the Prostate, Testicular, and Penile Oral Abstract Session at the 2021 American Society of Clinical Oncology 2021 Annual Meeting, Dr. Yamoah presented the results of the VanDAAM study (NCT02723734), a prospective study validating the genomic classifier to identify patients with a high risk of metastasis among African American men with early localized prostate cancer.
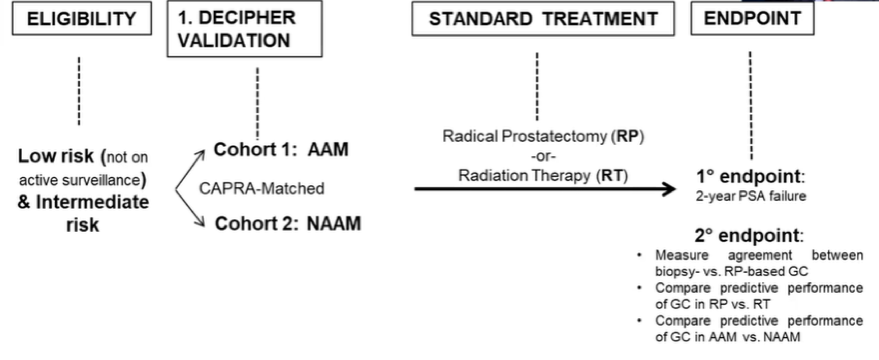
To do so, the authors performed a multisite, prospective validation trial of the genomic classifier (Decipher score) in African American men. Patients with low and intermediate risk prostate cancer were recruited, though those undergoing active surveillance were ineligible.
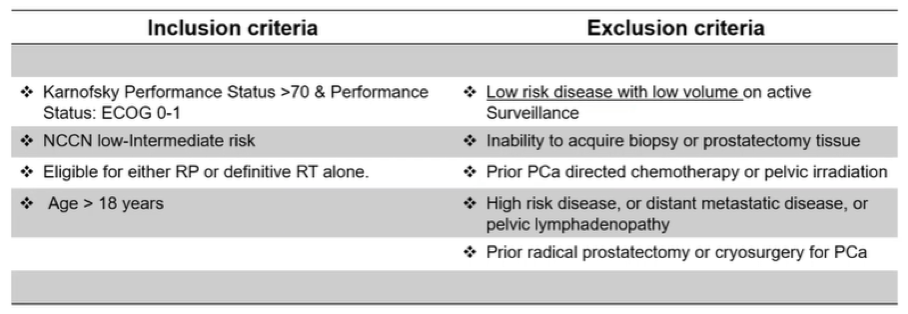
The authors performed enrollment with a 1:1 ratio of African American to non-African American men, matched on clinical characteristics including PSA, age, biopsy Gleason score, clinical stage, and percent positive biopsy cores.

The diagnostic biopsy specimens were processed at a CLIA certified laboratory. The Decipher score (GC) was calculated using a whole transcriptome profiling platform. The authors examined the risk of group migration between NCCN risk group and genomic classifier by race and then examined the relative risk of metastasis was estimated using negative binomial model. While the study is designed to assess the primary endpoint of two-year failure free survival following radical prostatectomy or radiotherapy, these data are immature and instead the authors focused their presentation on their secondary outcomes.
Finding that there was significant overlap between patient reported, self-identified race and genomically-derived ancestry, the authors utilized self-identified race for the purpose of analysis.
The authors accrued 207 evaluable men of an initial target accrual of 250 men, including 102 African American men and 107 non-African American men with comprehensive genomic information. On the basis of biopsy Decipher score, enrolled men were characterized as low, favorable, and unfavorable intermediate risk prostate cancer on the basis of their risk of metastasis. African American and non-African American men were well matched on the basis of clinical characteristics (apart from a younger age at diagnosis among African American men). Perhaps not surprisingly then, treatment selection did not differ between racial groups. However, among African American men, rates of histologic upgrading from biopsy to radical prostatectomy specimen was significantly more common (p=0.01).
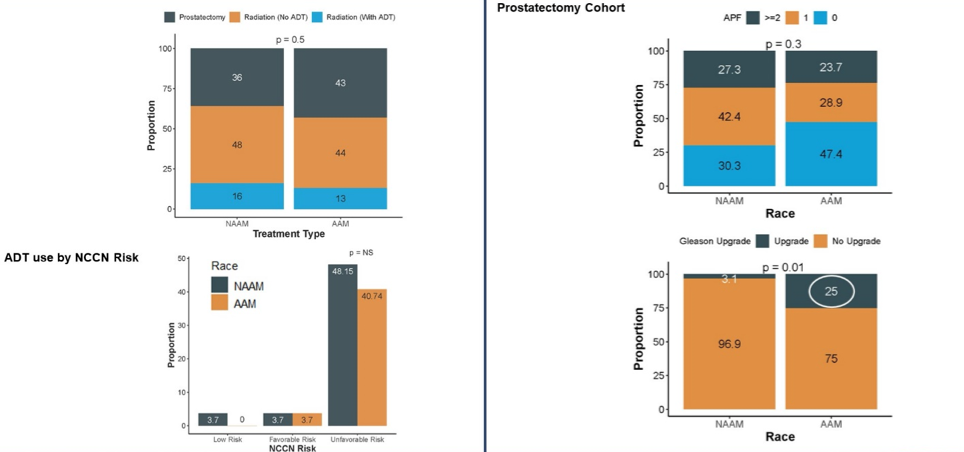
When stratified by clinicopathologically defined risk groups, there was significant genomic heterogeneity between African American and non-African American men across NCCN risk groups. Among patients with low or favorable intermediate risk disease based on clinical characteristics, African American men were much more likely to harbor high genomic risk tumors (49%), compared to only 10% of those in non-African American men (p = 0.02).
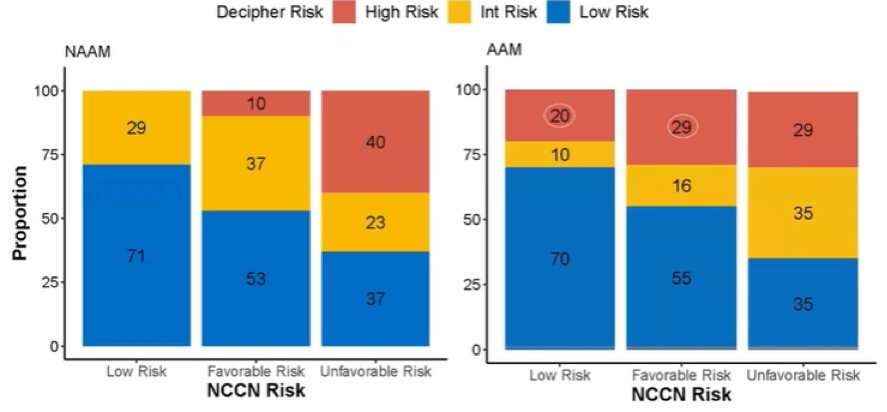
The authors further considered a metric of extreme deviation as a result of the incorporation of the Decipher information with clinicopathologic details, defined as extreme where there was “change in treatment recommendation”. A higher proportion of African American men experienced this extreme deviation in risk status (26.8% vs 8.1%, p=0.03). In a binomial model, African American men with low-favorable NCCN risk disease were 3.9 times (95% CI, 1.15 – 13.86, p = 0.02) more likely to be reclassified as high genomic risk for distant metastasis compared to non-African American men.

The authors further assessed the agreement in Genomic risk between prostate biopsy and radical prostatectomy specimens, finding good agreement in both African American men and non-African American men.
The authors concluded that standard clinicopathologic assessment using NCCN criteria often provides suboptimal risk stratification for African American men with prostate cancer. However, there is good concordance between biopsy and radical prostatectomy derived Decipher score regardless of race which supports the reliability of using biopsy derived specimens. Including the genomic risk classifier with clinical features may help to address disparities in prostate cancer outcomes in African American men.
Presented by: Kosj Yamoah, MD, PhD, Radiation Oncologist, Moffit Cancer Center
Written By: Christopher J.D. Wallis, MD, Ph.D., Urologic Oncology Fellow, Vanderbilt University Medical Center, Twitter: @WallisCJD at the 2021 American Society of Clinical Oncology (ASCO) Annual Meeting #ASCO21, June, 4-8, 2021

