The authors utilized the American Urological Association Quality (AQUA) Registry to identify 3,165 (̃ 25%) of US urology providers, representing 48 states and territories. The AQUA Registry collects data via automated extraction from electronic health record systems. They examined trends in prostate cancer care delivery from 156 practices contributing data in 2019 and 2020. Among patients diagnosed with prostate cancer, risk stratification was based on prostate-specific antigen (PSA) at diagnosis, biopsy Gleason, and clinical T-stage. The authors used a natural language processing algorithm to determine Gleason and T-stage from unstructured clinical notes.
The primary outcome of interest was the mean weekly visit volume by prostate cancer patients per practice (visits defined as all MD and mid-level visits, telehealth, and face-to-face), and we compared each week in 2020 through week 44 (November 1) to the corresponding week in 2019.
The authors identified 267,691 patients with prostate cancer in the AQUA registry who received care between 2019 and 2020. Comparing trends from mid-March to early November 2020 (week 10 – week 44), they observed differences in the magnitude of the decline and recovery between risk groups, with the greatest effect observed among patients with low-risk disease.
For the first nine weeks of 2020, overall mean visits per day (averaged weekly) were similar to 2019. However, over the subsequent 5 weeks (to week 14) there were large decreases in the number of visits (31% decrease relative to 2019 for patients with low-risk disease). Subsequently, there was a recovery of the number of prostate cancer-related visits, though as the of the cut-off for this analysis (week 44 of 2020), the mean number of prostate cancer-related visits remained much below the baseline rate. Thus, following an initial recovery by mid-year, there was a secondary decrease in the second half of 2020, relative to 2019.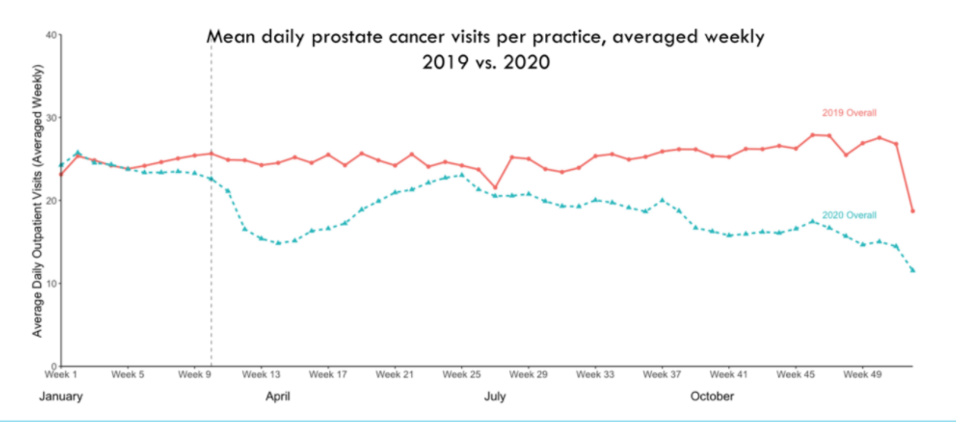
The authors then performed stratified analysis according to disease characteristics, demonstrating the most profound effects for patients with low-risk disease (a decrease of 46%).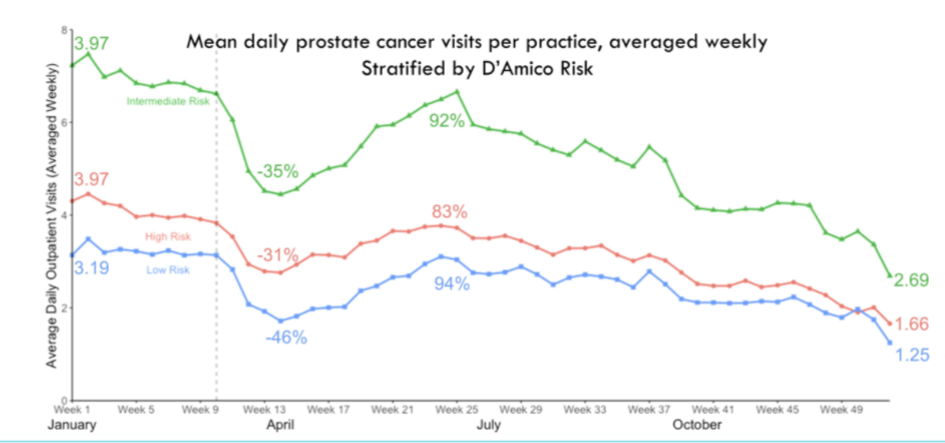
The authors then assessed for variation in trends in prostate cancer-related visits according to sociodemographic variation, demonstrating particularly significant effects among older individuals (age 65 years and older). Additionally, there were significant racial disparities with larger decreases for African American and Asian patients than Caucasian patients. The subsequent rebound was greater for Asian than African American patients.
They further examined specific procedures. In terms of prostate biopsy, there was a large drop-off in the average daily biopsies (assessed weekly) though 2020 rates returned to 2019 levels by July 2020. Radical prostatectomy and radiotherapy demonstrated a dramatic decrease in case volumes though recovery was much quicker. However, unlike prostate biopsy, there were significant secondary declines in both of these treatment modalities following initial recovery. The effect of androgen deprivation therapy was much less pronounced.
The authors conclude that the COVID-19 pandemic sharply decreased access to care for men with prostate cancer, with a differential effect according to disease risk (with a greater effect among those with low-risk disease) and with disparities between racial groups. To what extent these changes will affect cancer-related outcomes remains to be assessed.
Presented by: Matthew R. Cooperberg, MD, MPH, Professor of Urology; Epidemiology & Biostatistics, Helen Diller Family Chair in Urology, UCSF
Written by: Christopher J.D. Wallis, MD, Ph.D., Urologic Oncology Fellow, Vanderbilt University Medical Center, Twitter: @WallisCJD at the 2021 American Society of Clinical Oncology (ASCO) Annual Meeting #ASCO21, June, 4-8, 2021


