To frame the discussion, Dr. Carthon provided the case of an 81-year-old man with a history of Gleason 4+3=7 prostate cancer who was initially diagnosed in 2005 as a result of urinary symptoms, without PSA screening. He declined surgery at the time of diagnosis, stopped radiotherapy after a single fraction, and further deferred any additional therapy due to side effects and travel concerns. For many years, he had no prostate cancer follow-up. More recently, he was admitted to the hospital due to confusion and was diagnosed with both sepsis and widespread metastatic prostate cancer. Dr. Carthon suggested that we can consider several points regarding how care may have been improved, the role of medical mistrust in his delayed care, how patient navigation may affect his treatment choices.
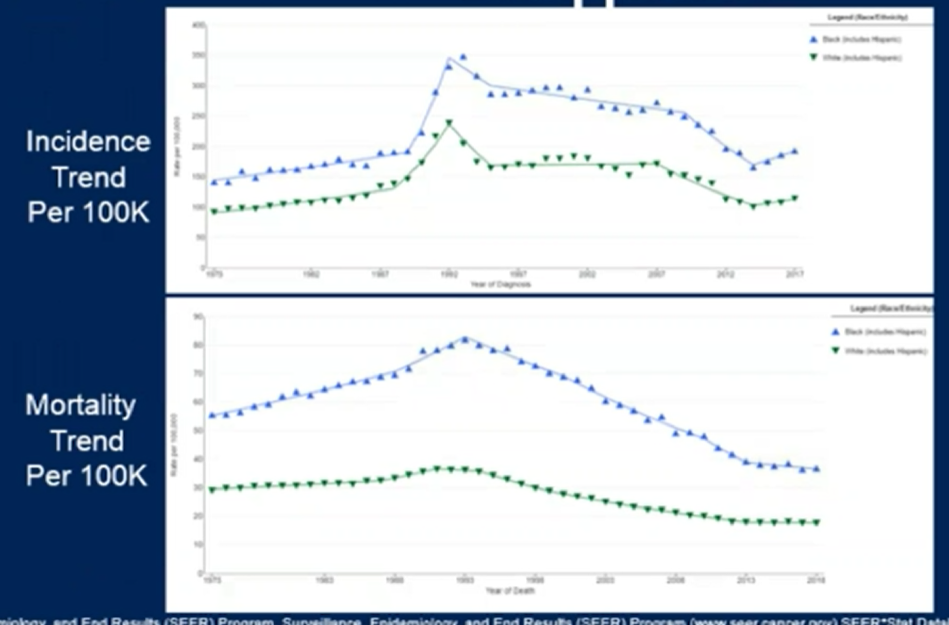
Dr. Carthon began by highlighting that there may be many underlying causes of health care disparities, including race, socioeconomics, education, and geography. While prostate cancer disparities have narrowed over time, they have not disappeared. Notably, the mortality gap between White and Black men widened during the initial periods of uptake of PSA screening, with subsequent decreases more recently. However, Black men remain more likely to die of prostate cancer.
In addition to race-based disparities, there is a strong influence of socioeconomics. However, in prostate cancer, White men appear to do similarly whether they are from poor or affluent counties. In contrast, Black men from affluent counties do worse than even poor White men. There has been significant interest therefore to examine variation in life expectancy between regions based on socioeconomics – recent work from the Atlanta area highlighted a 25-year difference between the wealthiest and poorest regions. He emphasized that cancer care likely contributes significantly to these differences as cancer is a leading cause of death.
Moving into 2021, it’s hard to understate the importance of the COVID-19 pandemic. Decreasing physician visits have affected cancer screening rates, with a 65% decrease in PSA screening during the pandemic. As a result, prostate cancer diagnoses have dropped approximately 25%. Prior work has shown that decreased screening, based on public health recommendations in 2012, resulted in later increases in locally advanced and metastatic disease at presentation. Thus, there are concerns that decreases in screening associated with the pandemic may result in a subsequent diagnosis of more advanced disease.
He then transitioned to highlight that patient navigation may be helpful. Among patients with abnormal PSA screening tests, the assistance of a patient navigator was associated with a more timely diagnosis of prostate cancer or the resolution of a benign finding. Thus, along the continuum from screening, through prostate cancer treatment, and follow-up, Dr. Carthon suggested that it may be prudent to increase access to patient navigators.
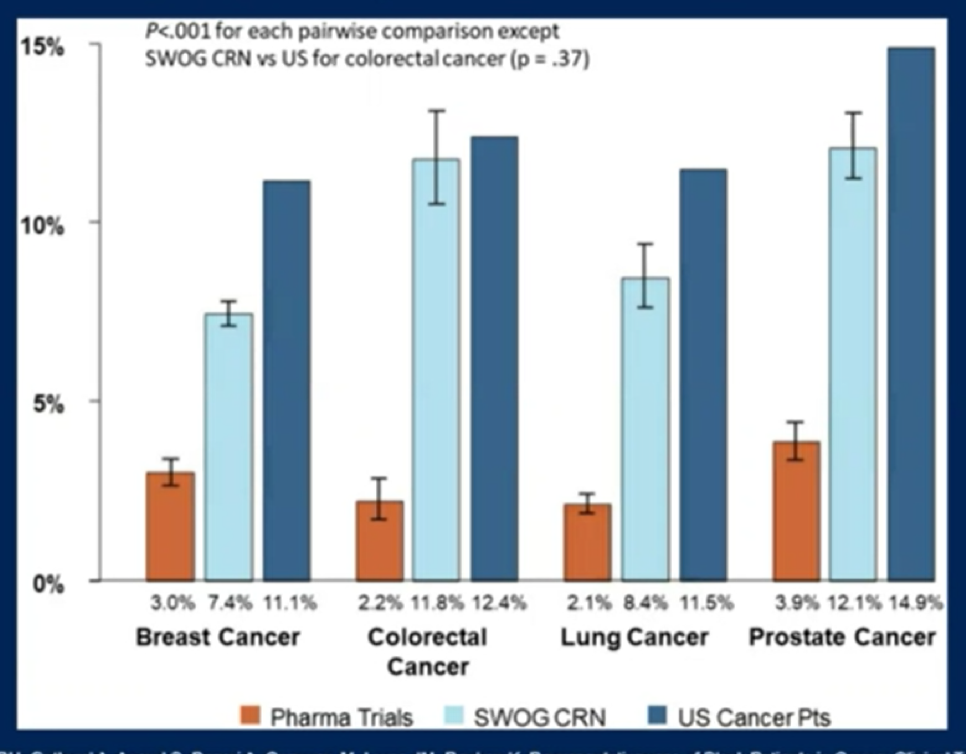
Dr. Carthon then transitioned to discussing the representation of Black patients in clinical trials.T his is particularly profound among pharmaceutical company-sponsored trials: while 15% of patients with prostate cancer are Black, less than 4% of patients on pharmaceutical company-sponsored trials are Black. Rates are somewhat better in cooperative group trials but still lags.
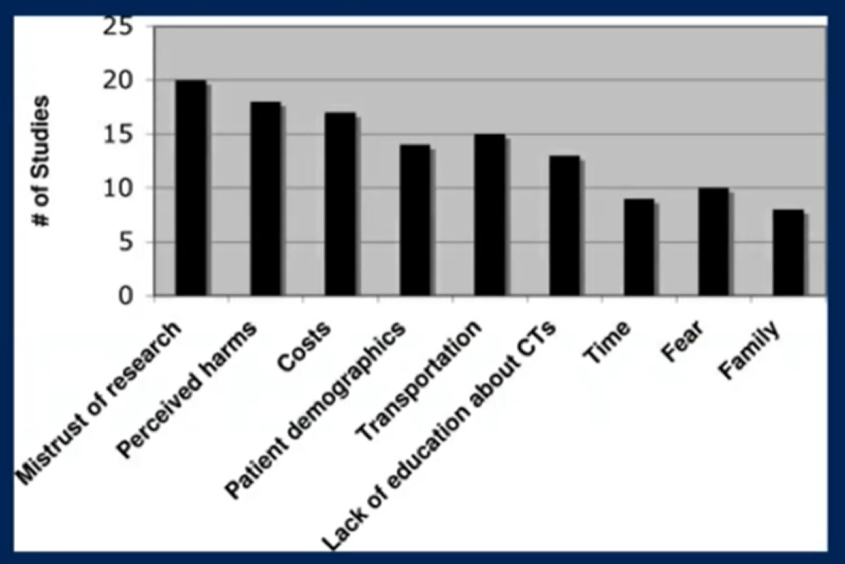
In addition to systemic issues, he highlighted that there are patient-driven factors that prevent patients from enrolling in trials. These include a mistrust of research, perceived harms, costs, and many others.
He then highlighted that, during the COVID pandemic, there has been a decentralization of cancer care and clinical trials, with an increased use of satellites. These newer models may be more flexible and allow collaboration with local clinicians, laboratories, and imaging facilities which may address many of the barriers highlighted above.
Dr. Carthon then discussed real-world evidence regarding the use of genomic analyses in a single institution cohort of patients with prostate cancer based on CTC analysis. This cohort was relatively highlight enriched with Black men compared to most study cohorts. The authors found that 30% of patients had changes in management as a result of testing.
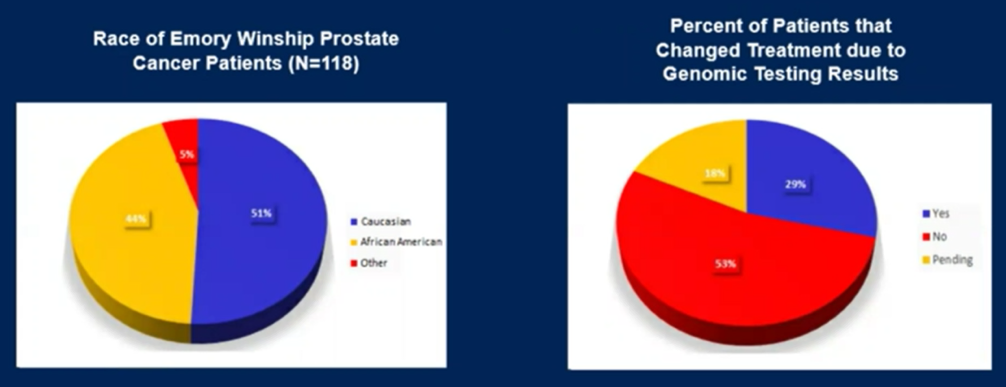
Black patients in this cohort presented at a younger age, with worse performance status, and with more advanced disease. Despite this, overall survival was similar between White and African American men.
He then suggested several strategies to improve outcomes in a diverse environment:
- Widespread prevention and screening, facilitated by education and patient navigation
- Equal access care environments and treatment opportunities.
- Accessibility to clinical trials, including decentralization to reduce barriers to involvement
- Systematic use of genetic testing, as suggested by guidelines.
Presented by: Bradley Curtis Carthon, MD, PhD, Associate Professor, Department of Hematology and Medical Oncology, Emory University School of Medicine, Section Chief of Hematology and Oncology, Emory University Hospital Midtown
Written by: Christopher J.D. Wallis, Urologic Oncology Fellow, Vanderbilt University Medical Center Contact: @WallisCJD on Twitter at the 2021 American Society of Clinical Oncology (ASCO) Annual Meeting, Virtual Annual Meeting #ASCO21, June, 4-8, 2021


