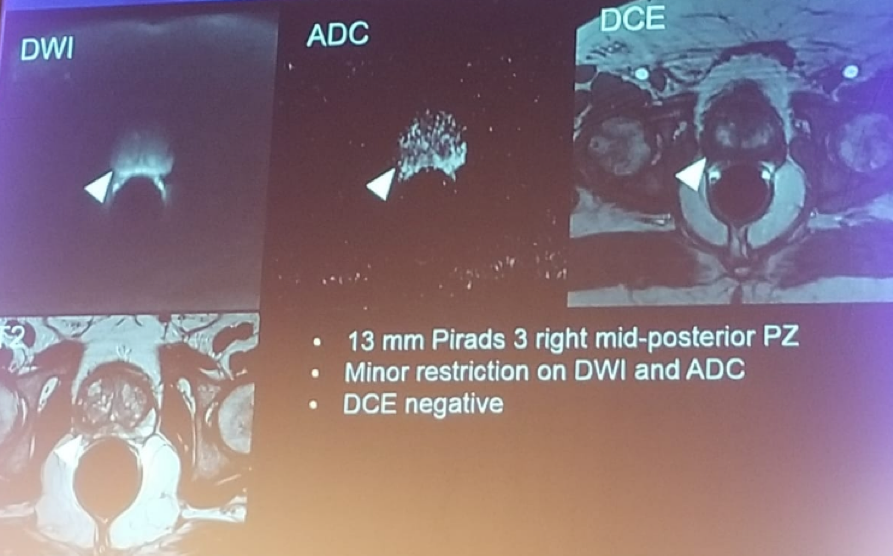
Figure 1 – Patient prostate MRI:
In the next section of this session, each of the panelists gave a short discussion on his proposed therapeutic strategy, and finally, the audience needed to vote and decide which treatment strategy they prefer.
1.The first Speaker was Claude Abbou, MD, France proposing robotic-assisted radical prostatectomy (RARP). Approximately 25% of patients with Gleason 3+4 low volume disease, undergoing surgery, will have adverse pathological findings.
According to Dr. Abbou, RARP is a one-day surgery, and the patients retain the catheter for one week only. According to the PIVOT trial, surgery was associated with less treatment for disease progression.1 Retrospective data have shown that survival rates are better with surgery compared to radiotherapy in intermediate risk disease.2
Potency rates at 6 months are approximately 87.9% and at 12 months 93.2%, with positive surgical margins in 9% of cases. Continence rates are excellent with 0.7% of patients undergoing RARP requiring a procedure for incontinence. According to the NCCN guidelines active surveillance (AS) is not recommended for intermediate-risk disease. The PROTECT study demonstrated that metastases and disease progression were more common in the active monitoring group than in the surgery or radiotherapy group.
Radiotherapy is not a good option as it entails high risk of complications if lower urinary tract symptoms exist. Previous data have shown a high relapse for radiotherapy as monotherapy and added toxicity when androgen deprivation therapy (ADT) is added.
Lastly, the limitations of focal therapy were discussed. First, PC is a multifocal disease in more than 50% of cases, so focal therapy will simply not treat all disease sites. Second, there is an issue with the accuracy of localization, and limited follow-up and long-term oncologic data. The EAU guidelines state that focal therapy is an investigational modality at this point.4 In vascular targeted phototherapy (VTP), the conversion rate of radical therapy is almost 24%. Biopsy results were positive in 50% vs. 86% after surveillance. Dr. Abbou concluded his short talk stating that RARP is still a gold standard for localized PC, and that the side effects of other procedures and 2nd line optional therapies are very poor.
2. The 2nd speaker was Derya Tilki, MD proposing open radical prostatectomy (RP). According to her, two randomized controlled trials (SPCG4 and PIVOT) have shown an overall survival (OS) benefit for open surgery when compared to watchful waiting, with 31% relative reduction in all-cause mortality. Dr. Tilki discussed the option of focal therapy, stating that the failure-free survival is 88% and metastasis-free survival is 98% at 5 years. However, only 1/3 of patients undergo a post-treatment biopsy, and therefore the true rate of persisting and/or recurrent cancer in these patients is unknown.5 She next discussed external beam radiotherapy (EBRT), that is an effective treatment option for favorable intermediate PC but with more adverse effects. Brachytherapy should be offered only to patients without a history of TURP, and with good IPSS and prostate volume less than 50 ml. Lastly, she discussed AS, but recent evidence suggests that any grade 4 pattern is associated with a 3-fold increased risk of metastases compared to Gleason 6. According to current EAU guidelines, there isn’t any sufficient evidence to support AS in the intermediate risk group.
Dr. Tilki concluded her talk, stating that radical prostatectomy is the preferred treatment option in this fit patient presenting with an IPSS of 12.
3. HIFU was discussed by Neil Fleshner, MD from Princess Margaret Cancer Center. Dr. Fleshner began by stating that our goal of trifecta should be very clear:
- Cancer (PSA) control - the patient will not die from PC
- A continent with normal urinary function
- Potent with preservation of erectile function
The advantages of focal therapy are that the dominant nodule, which is the most significant one, will be treated, and has been proven to cause all metastatic lesions. The disadvantages of this modality are the fact that PC is many times a multifocal disease, and not all lesions will be treated.
The procedure itself is easy and very effective, creating “popcorn” effects in the treated region (Figure 1). Contemporary outcomes of HIFU treatments for PC have shown recurrence rates of 8-16% at 1 year, with continence rates of 90-100%, and potency rates of 89-95%.6
Fleshner then presented the Princess Margaret experience of 166 focal therapy cases, with a follow-up of 24.3 months. 52% biopsied, 42% positive, 22% of the entire cohort. The medially located tumors are at higher risk of failure. Continence rates were 94.9%, no change in erectile function was noted in 86.5% of cases. Lastly, 84.1% had unchanged lower urinary tract symptoms. A total of 16 patients underwent a repeat HIFU, with 50% cleared the 2nd time, and adverse events were insignificant.
In conclusion, for the presented patient, there is 80-90% chance of being clear of cancer with HIFU, 90-95% chance of no ED, 90-95% with urinary preservation, and minimal chance of altering salvage options, if required.
Figure 1 – HIFU therapy – popcorn effect:

4. Bernard Malavaud, MD presented his treatment of focal cryotherapy. According to Dr. Malavaud, the percentage of pattern 4 is much lower than the biopsy demonstrates, and if it is 5% only pattern 4, it can basically be regarded as Gleason 6 (3+3) according to him. The presence of aggressive features is therefore questionable.
The choice of active surveillance has a psychological burden which must not be taken lightly. Anxiety over the uncertainty of the future or fear of losing the opportunity for a cure is an important driver of treatment. Therefore, the right treatment choice should be a focal treatment of the dominant lesion and active monitoring of the rest of the gland. Any other option, according to Dr. Malavaud could be deemed excessive in terms of sacrificing the gland and enduring adverse effects and is adventurous and with a significant cost.
Cryotherapy is a validated modality for precise tissue ablation (Figure 2) and should be the focal treatment of choice according to Dr. Malavaud.
Figure 2 – Cryotherapy:
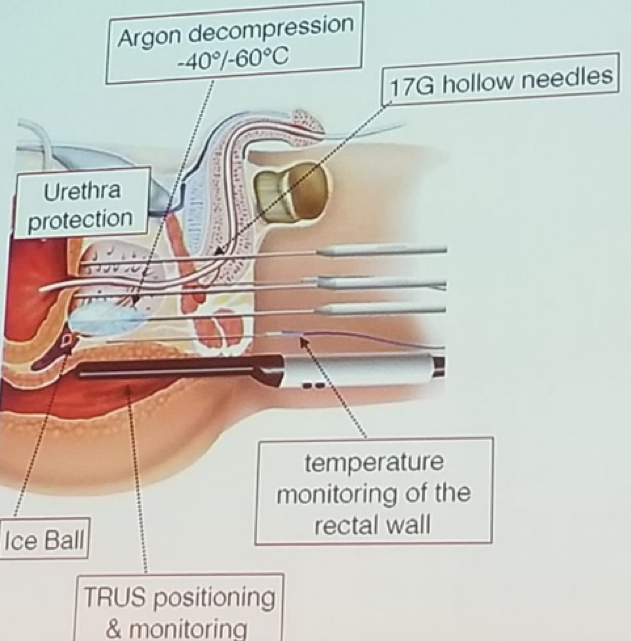
5. Dr. Coleman from MSKCC presented his option of vascular targeted photodynamic therapy (VTP). The available therapeutic options for this patient include AS, partial gland ablation, surgery, and radiotherapy. For partial gland ablation, the approved options include VTP (TOOKAD), HIFU, and Cryotherapy. Since the tumor is posterior, next to sensitive adjacent structures such and nerves and rectum, cryotherapy with its resulting ball of ice, is not a good option, as it will damage the nerve and rectum in order to reach a lethal tumor temperature. In HIFU there will be near field cavitation effects, and poor acoustic energy with rectal wall heating, leading to nerve damage and rectal injury.
In VTP (TOOKAD) a light-sensitive agent is activated in the prostate by laser fibers (inserted transperineally) using near-infrared light. This produces non-thermal coagulative tissue necrosis by localized free-radical mediated effects. It is an effective cancer ablation treatment in both animal and human studies. There has been extensive rigorous testing for localized PC all over the world, in phase 1,2, and 3 studies. It has also been proven that it feasible to salvage prostates treated with VTP without any significant issues, with minor to no complications and a continence rate of 95% and potency of 53%.
In conclusion, based on evidence, VTP therapy is the best focal therapy to date, suited to patient anatomy, with no impact on function, approved in Gleason 3+4 disease, effective, safe and salvageable, and equally effective in all sites.
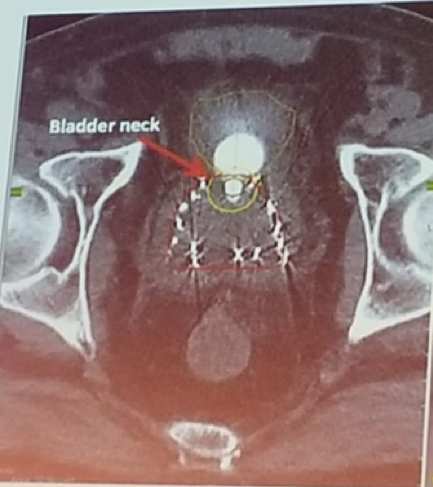
6. Dr. Zvi Symon presented his view on using brachytherapy for this patient. For patients with a favorable intermediate-risk disease, such as this patient, brachytherapy alone is an excellent option, according to the NCCN guidelines.7 According to studies, there is no difference in oncological outcomes between brachytherapy alone and the combination of brachytherapy + External Beam radiotherapy (EBRT).8 If the patient does have some lower urinary tract symptoms, it is preferable that the patient start taking alpha blockers, have their IPSS re-evaluated, and be treated with LDR seed implant. Brachytherapy is a simple day procedure, where patients can go home the same day and can be physically active the following day. The bladder neck is a sensitive are, prone for radiation toxicity (figure 3), that careful attention must be paid before and during treatment.
Figure 3 – Brachytherapy and bladder neck:
7. Lastly, Laurence Klotz, MD gave his perspective on using active surveillance (AS) in this patient. He began with the key points favoring AS over other treatments. Surgery and radiation have too many adverse effects, and in focal therapy, there are too many unanswered questions. Unfortunately, there is no long-term data on outcomes of focal therapy, concern about the effects of sub-lethal treatment on disease progression – ‘accelerated re-population’. There is uncertainty about patient selection and treatment parameters, and in addition, salvage treatment may be compromised. However, these patients have ‘wiggle room’ allowing for additional tests to be done, including MRI, biomarkers, which will allow us to identify the good and bad actors.
The next topic discussed was the fact that AS is offered for a Gleason 3+4 disease. In the well-known CAPRA score for stratifying PC risk (low – 0-2, intermediate -3-5, and high – 6-10), a Gleason of 3+4 adds only one point to the score, compared to Gleason 3+3. Furthermore, a minimal quantity of Gleason pattern 4 on biopsy is associated with a low-risk tumor in RP specimen, and there has been no difference in the distribution of RP grade or pathological T stage between biopsy Gleason 3+3 and 3+ pattern 4 less than 5%. [9] The PROTECT study had shown no difference in cancer-specific survival and progression-free survival between treatment and AS in these specific patients.3
In conclusion, the presence of pattern 4 Gleason confers an increased risk of metastases compared to Gleason 3. However, the intermediate risk cancer covers a broad range of risk. Tools exist to stratify patients and they should be used (MRI and biomarkers). In those with favorable parameters, expectant management has a compelling quality of life advantages.
At the conclusion of this debate, the audience voted for Dr. Klotz presenting AS, as the most suitable option for this patient.
References:
1. Wilt TJ. Et al. NEJM 2017
2. Marsh S et al. Clin Genitourinary Cancer 2017
3. Hamdy F et al. NEJM 2016
4. Van der Poel H. et al. BJUI Int 2018
5. Murphy D. et al. Eur Urol 2018
6. Ernesto R et al. European Urol 2015
7. Chin J. et al. JCO 2017
8. Markovic ES et al. BJUI 2018
9. Huang C. et al. American Journal of surgical pathology 2014
Speakers:
Robotic RP: Claude Abbou, MD, France
Open RP: Derya Tilki, MD, Germany
Focal HIFU: Neil Fleshner, MD, Canada
Focal Cryo: Bernard Malavaud, MD, France
Vascular Targeted Therapy: Jonathan Coleman, MD, USA
Brachytherapy: Zvi Symon, MD, Israel
Active Surveillance: Laurence Klotz, MD, Canada
Written by: Hanan Goldberg, MD, Urologic Oncology Fellow (SUO), University of Toronto, Princess Margaret Cancer Centre @GoldbergHanan at the 2018 FOIU 4th Friends of Israel Urological Symposium, July 3-5. 2018, Tel-Aviv, Israel


