TA was traditionally reserved for older and/or frail patients, yet more recent data has demonstrated strong functional and oncologic outcomes for TA for patients with SRM.1 The current AUA guidelines now state that TA can be considered a reasonable alternative management strategy even in healthy patients with SRM.2 However, previous studies have suggested that local oncologic control may not be as strong with TA, and how this plays out in the high-stakes situation of RMSK remains unclear.3,4 Moreover, comparative functional and oncologic outcomes between PN and TA are not well defined for patients with RMSK.
To address these issues, we recently reviewed our institutional experience with cT1 RMSK (1975-2022) with 409 patients managed with PN and 95 managed with TA.5 Our objective was to compare the functional and oncologic outcomes between these two modalities. We utilized a 1:1 propensity score to match the cohorts with respect to patient age, sex, preoperative GFR, body mass index, comorbidity status (i.e., hypertension, diabetes, and cardiovascular disease), R.E.N.A.L., and tumor diameter. Overall, the matched cohort included 132 patients (TA=66 and PN=66). For the matched cohort, the median age was 68 years, and 69% were male. The median preoperative GFR was 51 mL/min/1.73 m2. Median tumor size and R.E.N.A.L. were 2.4 cm and 6, respectively, and median follow-up was 41 months in the PN cohort and 59 months in the TA cohort.
Overall, TA was associated with modestly improved functional outcomes compared to PN, but local disease control was not as strong for TA. PN was associated with greater than five-fold higher rates of acute kidney injury, and TA preserved a median of 89% of the preoperative GFR compared with 83% for the PN cohort (p<0.05). However, the long-term functional outcomes and dialysis-free survival rates were similar between the two groups. Regarding oncologic outcomes, five-year recurrence-free survival was reduced after TA compared with PN (62% vs 86%, p<0.05). Local recurrence was found in fourteen patients after TA and was not always salvageable with nephron-sparing modalities. Two of these fourteen patients required RN. For the twelve patients managed with salvage TA, there were five systemic recurrences. In three of these patients, local control could not be regained with salvage TA. Cancer-specific survival was comparable between the two modalities although longer follow-up will be required to assess this more rigorously (See Figure).
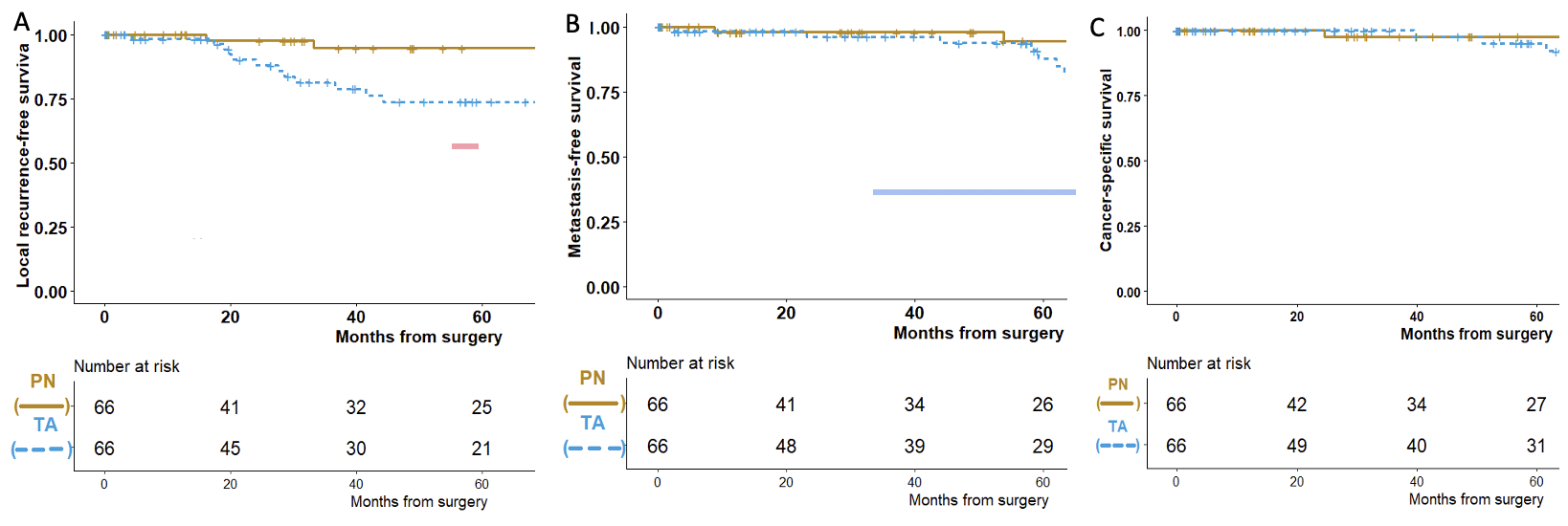
Figure: Kaplan-Meier survival estimates for patients with cT1 tumor in a solitary kidney managed with thermal ablation (blue/dashed) or partial nephrectomy (gold/solid). A) Local recurrence-free survival based on the initial ablation, log-rank, p<0.01; B) Metastasis-free survival, log-rank, p=0.07; C) Cancer-specific survival, log-rank, p=0.7
Our study highlights the importance of careful patient selection when considering TA for patients with RMSK. Current AUA guidelines recommend that TA can be selectively considered even in healthy patients with SRM.2 These recommendations are made with the assumption that salvage TA will lead to appropriate cancer-specific control and that other surgical management strategies (e.g., radical nephrectomy [RN]) are still on the table. However, RN is not a desired outcome for patients with RMSK and PN can be more challenging after TA in our experience.1,4 As such, it is critical to evaluate each individual patient to assess whether TA would be an appropriate management strategy. Nine of the fourteen patients (64%) who experienced local recurrence after TA in this series had multifocality and/or cT1b tumors suggesting that patient selection may not have been optimal. Local recurrence was also more often seen in patients with the older laparoscopic approach to TA compared to conventional percutaneous TA, highlighting the potential importance of the learning curve. With these considerations in mind, TA has evolved as a reasonable consideration for patients with SRM in a solitary kidney, presuming appropriate patient selection.

Written by: Carlos Munoz-Lopez & Steven C. Campbell, MD, PhD; Department of Urology, Glickman Urological and Kidney Institute, Cleveland Clinic
Co-Authors: Kieran Lewis, Eran Maina, Worapat Attawettayanon, Akira Kazama; Department of Urology, Glickman Urological and Kidney Institute, Cleveland Clinic
References:
- Kriegmair MC, Bertolo R, Karakiewicz PI, et al. Systematic Review of the Management of Local Kidney Cancer Relapse. Eur Urol Oncol. 2018;1(6):512-523.
- Campbell SC, Clark PE, Chang SS, Karam JA, Souter L, Uzzo RG. Renal Mass and Localized Renal Cancer: Evaluation, Management, and Follow-Up: AUA Guideline: Part I. J Urol. 2021;206(2):199-208.
- Fraisse G, Colleter L, Peyronnet B, et al. Peri-operative and local control outcomes of robot-assisted partial nephrectomy vs percutaneous cryoablation for renal masses: comparison after matching on radiological stage and renal score. BJU Int. 2019;123(4):632-638.
- Liu NW, Khurana K, Sudarshan S, Pinto PA, Linehan WM, Bratslavsky G. Repeat partial nephrectomy on the solitary kidney: surgical, functional and oncological outcomes. J Urol. 2010;183(5):1719-1724.
- Attawettayanon W, Kazama A, Yasuda Y, et al. Thermal Ablation Versus Partial Nephrectomy for cT1 Renal Mass in a Solitary Kidney: A Matched Cohort Comparative Analysis. Ann Surg Oncol.


