Urinary diversion (UD) is inevitable following RC, which carries certain risks including hyperchloremic metabolic acidosis and renal function decline that may occur in up to a third of patients.3
Several studies have identified age, diabetes mellitus, chronic hypertension, ureteroenteric anastomosis stricture, and pyelonephritis as independent risk factors of renal function deterioration after RC and UD.4 The impact of diversion type on renal function is not very clear, yet the majority of studies have shown similar postoperative GFR changes following RC with different UD including orthotopic neobladder (ONB) and ileal conduit (IC).5
A bladder substitution with the intestine can lead to an increase in acid load and metabolic abnormalities.6 Pre-existing renal insufficiency can exacerbate these metabolic disturbances and also brings some risks/limitation in patients undergoing RC and UD. Thus, adequate kidney function is believed to be necessary to mitigate the metabolic effects of continent diversions. It is generally recommended to have a creatinine clearance of at least 40 ml/min to receive ONB.7 Moreover, the exacerbation of existing kidney damage by metabolic abnormalities has also been deemed a possible risk.8 A recent study from our center showed that patients with chronic kidney disease (stage IIIa) who underwent ONB had a comparable postoperative kidney function to those with a GFR ≥ 60 ml/min.9
Due to the complex nature of RC surgery, it presents a unique opportunity for evaluating the outcome of single (functioning) kidney (SK) versus double kidney (DK) patients. The number of studies comparing the surgical outcomes of SK and DK patients is sparse. In this study, we evaluated the perioperative and functional outcomes of RC and UD in patients with a SK vs. DK.
Patients who underwent RC for bladder cancer at USC between 2004 and 2020 with a history of prior or concurrent nephrectomy were reviewed. Dialysis-dependent patients with chronic kidney disease were excluded. With 2:1 matching, postoperative GFR of the SK group were compared with those of the DK group following RC. A total of 186 RC patients were included; 62 SK, and 124 DK. Among the SK patients, half (31/61) underwent continent UD, including 28 neobladders and 3 continent cutaneous UD.
A higher median length of hospital stay was observed in the SK group (8 days compared to 6 days, P = 0.006). Nevertheless, the rates of 90-day complications, readmissions, and mortality were similar between the groups. Patients with continent diversion showed similar 90-day complications between SK and DK (71% vs. 69%, P = 1.0), including metabolic acidosis and dehydration. Additionally, high-grade complications within 90 days were also similar (15.3% vs. 23.7%, P = 0.41) as well as 90-day mortality (4.8% vs. 1.6%, P = 0.43).
A significant difference in GFR changes was observed between the SK and DK groups at discharge, three and twelve months after RC (Fig. 1). Despite this, no significant difference was observed in postoperative GFR range in SK patients with continent or incontinent UD (Fig. 2). A multivariable analysis found no association between UD (continent vs. incontinent) and %post-operative/baseline GFR change at discharge, 3 and 12 months following RC (P = 0.61, P = 0.12, P = 0.41).
This study concludes that perioperative outcomes of radical cystectomy patients with single kidney are similar to those of double kidney patients, with the exception of a greater decline in GFR in single kidney patients. Single-kidney patients can undergo continent urinary diversion just as safe as those with double kidneys.
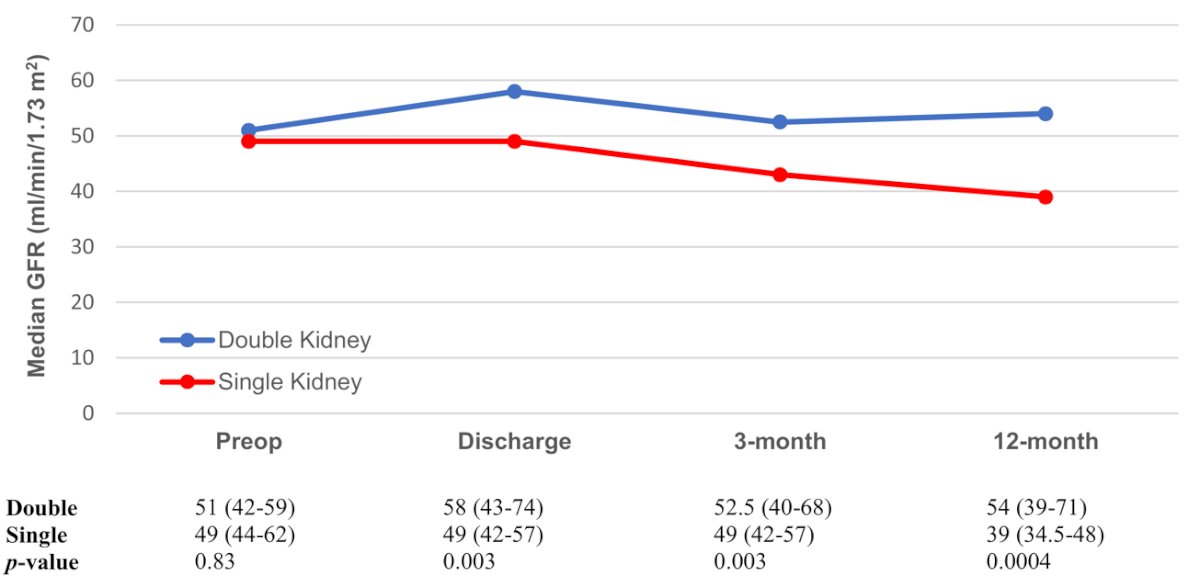
Fig. 1. GFR changes in patients undergoing radical cystectomy with urinary diversion, stratified by kidney status (single vs. double).
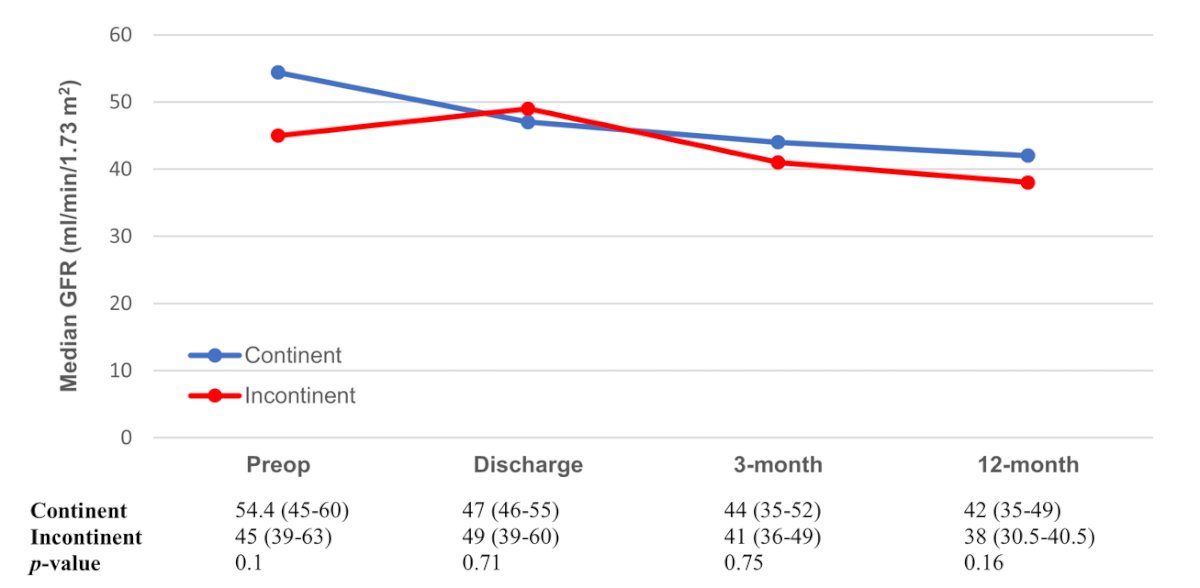
Fig. 2. GFR changes in SK patients undergoing radical cystectomy, stratified by type of urinary diversion (continent vs. incontinent).
Written by: Farshad Sheybaee Moghaddam, MD & Hooman Djaladat, MD, MS, Institute of Urology, Norris Comprehensive Cancer Center, University of Southern California, Los Angeles, California
References:
- Lowrance WT, Rumohr JA, Chang SS, Clark PE, Smith JA, Jr., Cookson MS. Contemporary open radical cystectomy: analysis of perioperative outcomes. J Urol. 2008;179(4):1313-8; discussion 8. Epub 20080304. doi: 10.1016/j.juro.2007.11.084. PubMed PMID: 18289578.
- Shabsigh A, Korets R, Vora KC, Brooks CM, Cronin AM, Savage C, et al. Defining early morbidity of radical cystectomy for patients with bladder cancer using a standardized reporting methodology. Eur Urol. 2009;55(1):164-74. Epub 20080718. doi: 10.1016/j.eururo.2008.07.031. PubMed PMID: 18675501.
- Osawa T, Shinohara N, Maruyama S, Oba K, Abe T, Maru S, et al. Long-term renal function outcomes in bladder cancer after radical cystectomy. Urol J. 2013;10(1):784-9. PubMed PMID: 23504683.
- Sheybaee Moghaddam F, Ghoreifi A, Djaladat H. Comparative performance of the different orthotopic urinary diversions. Curr Opin Urol. 2022;32(5):554-60. Epub 20220715. doi: 10.1097/mou.0000000000001016. PubMed PMID: 35849718.
- Iqbal U, Houenstein HA, Elsayed AS, Jing Z, James G, Hussein AA, et al. Ileal conduit versus neobladder: A propensity score-matched analysis of the effect on renal function. Int J Urol. 2022;29(2):158-63. Epub 20211208. doi: 10.1111/iju.14747. PubMed PMID: 34879435.
- Krajewski W, Piszczek R, Krajewska M, Dembowski J, Zdrojowy R. Urinary diversion metabolic complications - underestimated problem. Adv Clin Exp Med. 2014;23(4):633-8. doi: 10.17219/acem/28251. PubMed PMID: 25166450.
- Lee RK, Abol-Enein H, Artibani W, Bochner B, Dalbagni G, Daneshmand S, et al. Urinary diversion after radical cystectomy for bladder cancer: options, patient selection, and outcomes. BJU Int. 2014;113(1):11-23. doi: 10.1111/bju.12121. PubMed PMID: 24330062.
- Jin XD, Roethlisberger S, Burkhard FC, Birkhaeuser F, Thoeny HC, Studer UE. Long-term renal function after urinary diversion by ileal conduit or orthotopic ileal bladder substitution. Eur Urol. 2012;61(3):491-7. Epub 20110915. doi: 10.1016/j.eururo.2011.09.004. PubMed PMID: 21944435.
- Ahmadi H, Reddy S, Nguyen C, Douglawi A, Ladi-Seyedian S, Roberts S, et al. Long-term renal function in patients with chronic kidney disease following radical cystectomy and orthotopic neobladder. BJU Int. 2022;130(2):200-7. Epub 20220127. doi: 10.1111/bju.15685. PubMed PMID: 35044045.


