BERKELEY, CA (UroToday.com) - In this paper we present the largest Australian series of artificial urinary sphincter surgery; 77 men implanted between 2007-2013. All were for stress urinary incontinence following prostate cancer treatment, with approximately half having undergone open radical prostatectomy, and most of the remainder, robotic assisted surgery. Our analysis specifically focused on the difference in outcomes between those who had received adjuvant or salvage radiotherapy (37.7%), and those who had undergone surgery alone. There is surprisingly little data on the impact of radiation on subsequent continence surgery, yet it is critical to understand the effect this has on restoring urinary control if we are to adequately counsel patients of the risks vs benefits of post-prostatectomy radiotherapy.
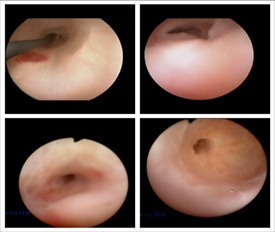 What was striking in our series was the high incidence of co-existing urethral strictures in men who had a history of radiation therapy (62.1 vs 10.4%). After radiation therapy these usually affect the membranous urethra (as opposed to the true anastomotic contracture seen after surgery alone), are often lengthy and complex, and occurring within a poorly vascularized urethra can be recalcitrant to endoscopic stabilization (see figure). In our experience this often became a crippling side-effect of prostate cancer treatment and significantly affected the management options available; particularly as definitive management via urethroplasty is generally not feasible given the length of stricture and surrounding ischaemic, irradiated tissue. In selected men with recurring strictures who may otherwise have been facing urinary diversion, we accepted the need for continued self-catheterization and interval dilatation, and proceeded with implantation. A transcorporal cuff placement was a particularly useful approach in these men to minimize the risk of urethral erosion.
What was striking in our series was the high incidence of co-existing urethral strictures in men who had a history of radiation therapy (62.1 vs 10.4%). After radiation therapy these usually affect the membranous urethra (as opposed to the true anastomotic contracture seen after surgery alone), are often lengthy and complex, and occurring within a poorly vascularized urethra can be recalcitrant to endoscopic stabilization (see figure). In our experience this often became a crippling side-effect of prostate cancer treatment and significantly affected the management options available; particularly as definitive management via urethroplasty is generally not feasible given the length of stricture and surrounding ischaemic, irradiated tissue. In selected men with recurring strictures who may otherwise have been facing urinary diversion, we accepted the need for continued self-catheterization and interval dilatation, and proceeded with implantation. A transcorporal cuff placement was a particularly useful approach in these men to minimize the risk of urethral erosion.
At a relatively short-term follow-up of 21.2 months, the continence rates (86.2 vs 86.5%), rate of cuff erosion (3.4 vs 2.0%) and revision surgery (10.3 vs 12.5%) were similar in both groups. In our experience, therefore, it seems the risk of delayed posterior urethral stricturing post adjuvant/salvage radiation may be higher than suggested in the radiation oncology literature, and this can significantly complicate subsequent continence management. However. these men can still be offered prosthetic surgery with a high chance of restoring urinary control.
Written by:
Daniel Moon, MBBS (Hon), FRACS (Urology) as part of Beyond the Abstract on UroToday.com. This initiative offers a method of publishing for the professional urology community. Authors are given an opportunity to expand on the circumstances, limitations etc... of their research by referencing the published abstract.
Director of Robotic Surgery
Epworth Healthcare, Melbourne, Australia
Outcomes of artificial urinary sphincter implantation in the irradiated patient - Abstract

More Information about Beyond the Abstract


