In this study, older adults starting one of three treatments for metastatic prostate cancer (chemotherapy, androgen-receptor axis targeted therapies (ARAT), or radium-223) at one of two comprehensive cancer centers in Toronto, Canada participated in RSM. Participants completed the Edmonton Symptom Assessment Scale (ESAS) online or by phone during the first cycle of treatment (3 weeks for patients starting chemotherapy and 4 weeks for those starting an ARAT (enzalutamide or abiraterone) or radium-223). The ESAS is a widely used cancer symptom screening tool that assesses 9 core physical and mental health symptoms on a scale from 0 (none) to 10 (worst possible). When patients rated their symptoms as severe (ESAS >7) or worsening symptoms (increased by at least 2 points), a more detailed questionnaire specific to the symptom was sent. If specific cut-offs scores suggesting severe symptoms were met, the nurse and oncologist were notified. Participants were also advised to visit the emergency department or contact a nurse at the genitourinary clinic of their primary hospital or an after-hours oncology nursing line.
Although RSM has demonstrated its success in improving quality of life and reducing hospitalizations in adult populations with cancer undergoing chemotherapy², it is not yet common practice. Given that RSM can be implemented using existing technology (automated telephone systems, emailed e-surveys, etc),² understanding whether it is feasible and acceptable among older adults; who may struggle with a digital interface compared to their younger counterparts; was the primary objective of this study. 90 participants completed the study with 34 undergoing chemotherapy, 43 an ARAT therapy, and 13 treated with radium-223. The average participant was aged 77 years, considered frail (58% scored greater than or equal to 3 on the VES-13), and were at least somewhat comfortable with using a smartphone or the internet. Response rates of over 90% were observed for both daily and weekly questionnaires. Most notifications sent to the oncology team (97%) were acknowledged, with 28% of cases resulting in consultation with a nurse, 15% resulting in medication counseling, and 9% resulting in a specialist referral. Outcomes such as an ER visit and consultation with an after-hours nurse were also observed but could not be fully captured in this study.
Table 1: Participant’s qualitative feedback regarding participating in daily remote symptom monitoring (RSM).
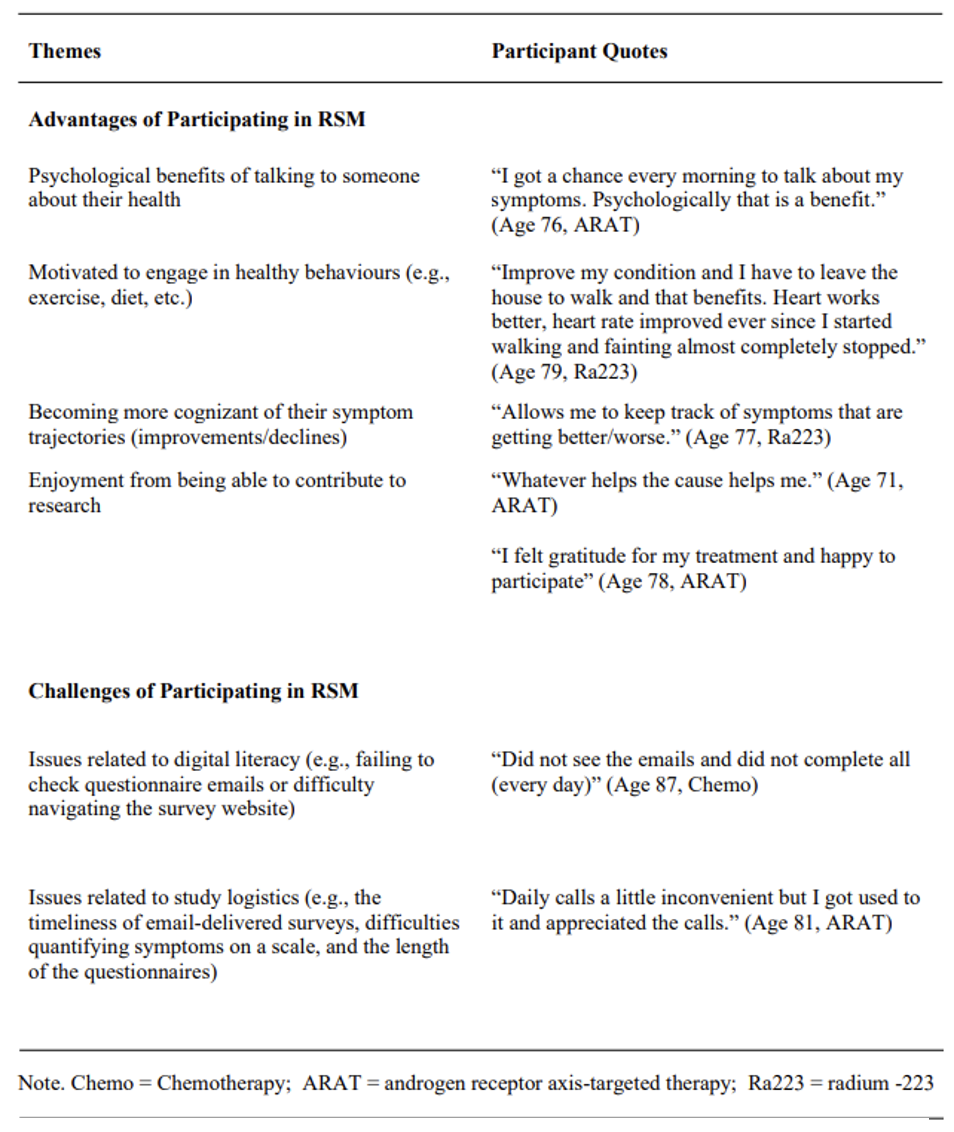
A 95% patient satisfaction rating was reported for the use of RSM, demonstrating the acceptance of RSM among older adults living with cancer. Most responders (66%) indicated that taking part in the study had advantages, such as the psychological benefits of talking to someone about their health, engaging in healthy behaviors, and becoming cognizant of their symptom trajectories. Participants also reported enjoyment in contributing to research as detailed in Table 1. Participants in the study also reported some challenges with digital literacy (e.g., failing to check questionnaire emails or difficulty navigating the survey website) as well as with study logistics (e.g., the timeliness of email-delivered surveys, difficulties quantifying symptoms on a scale, and the length of the questionnaires). These lessons begin to reveal how RSM can be adapted to fit the needs of older adults living with cancer.
There are also some limitations to this study. We did not explore patient-related health outcomes of RSM (e.g., treatment changes, healthcare use, etc.), which is necessary to determine the full utility of RSM. Since we did not conduct RSM outside of regular working hours and beyond one treatment cycle, this may have affected the outcome of alerts and completion/retention rates. Finally, although response rates for interviews were high, it is possible that participants who declined to be interviewed were less satisfied with the study. It is important to note that the short length of the intervention may have influenced response rates and is a key limitation. Therefore, further studies over longer periods are warranted to understand the applications of RSM in the geriatric oncology landscape.
Overall, RSM was shown to be a feasible and acceptable intervention for older adults undergoing cancer treatment. Although most participants opted for web-based monitoring, 38% preferred traditional telephone monitoring. As such, both web-based and phone-based operations should be considered when designing RSM interventions, which can not only be applied to older adults but to those undergoing various cancer treatments.
Written by: Sapeda R. Said Muhammad,1 Sanchiv Suresh,2 Gregory Feng,3 Milothy Parthipan,3 Henriette Breunis,4 Shabbir M.H. Alibhai4
- Research Student, University Health Network, Toronto, Canada.
- Research Assistant, University Health Network, Toronto, Canada.
- Department of Medicine, University Health Network, Toronto, Canada.
- Department of Supportive Care, Princess Margaret Cancer Centre, Toronto, Canada
- Side effects. Canadian Cancer Society. 2023. https://cancer.ca/en/treatments/side-effects. Accessed April 06, 2023.
- Basch E, Rocque G, Mody G, Mullangi S, Patt D. Tenets for implementing electronic patient-reported outcomes for remote symptom monitoring during cancer treatment. JCO clinical cancer informatics 2023;7.


