Our study included 626 biopsy-naïve men, between February 2015 and February 2018, after referral by their general practitioner in two community hospitals, one diagnostic center, and one university center.4 Men underwent prebiopsy contrast-enhanced mp-MRI. Prior to biopsy, two blinded expert readers subsequently assessed 1) “fast” bp-MRI (axial T2-weighted imaging (T2WI) with diffusion-weighted imaging (DWI)), 2) bp-MRI (triplanar T2WI and DWI), and 3) mp-MRI (triplanar T2WI, DWI, and dynamic contrast-enhanced (DCE) imaging). Thereafter, all men underwent systematic transrectal ultrasound-guided biopsies (SBs). In case of suspicious mp-MRI (PI-RADS 3–5 lesions), men also underwent MRGB.
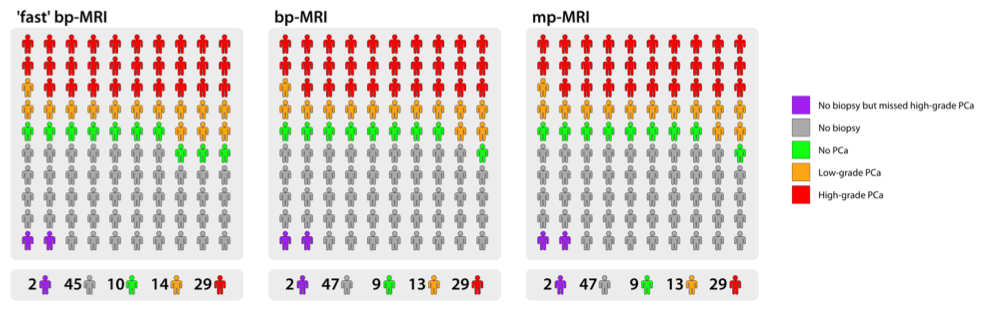
Our study showed that MRI acquisition time can substantially be reduced with faster, unenhanced bp-MRI protocols while maintaining the advantages of biopsy avoidance without impairing the detection of high-grade PCa. Both bp-MRI protocols had a similar diagnostic performance to that of mp-MRI with respect to “ruling out” high-grade PCa. Thus, the use of a “fast” bp-MRI protocol did not result in decreased detection of high-grade PCa (Figure 1).
Figure 1: MRI and histopathological results for each MRI protocol per 100 men
There are several important features of bp-MRI that facilitate clinical implementation of this technique. The noncontrast bp-MRI examination time is approximately 13 min, a reduction of 20% compared with mp-MRI. The “fast” bp-MRI protocol, without coronal and sagittal T2WI planes, can further reduce the acquisition time to 8 min. Therefore, patient throughput can be doubled to four men per hour. This increases accessibility while direct cost decrease. Additionally, intravenous access for contrast agent is not needed, therefore the procedure is noninvasive. Moreover, patients are not exposed to risks associated with contrast administration e.g. allergic reactions or nephrogenic systemic fibrosis.
There are, however, diagnostic compromises of the “fast” bp-MRI that have to be considered. It leads to ± 2% more biopsies and overdetection of ± 1% more low-grade PCa (ISUP Grade 1; Gleason score 3+3=6). We think this is mainly due to uncertainty in the assessment of some lesions to their zonal region (i.e. peripheral or transition zone). This resulted in an increased number of PI-RADS 3 (“equivocal”) lesions.
A potential limitation of our study is the high-quality image acquisition and expert reading of MRI, with a rather low percentage of PI-RADS 3 lesions. In lower-volume, nonexpert centers with more diagnostic uncertainty this might result in more unnecessary biopsies. Therefore, our results are not directly generalizable. In our opinion, this emphasizes the need for high-quality standards in image acquisition and standardized reading of prostate MRI.
In this study, both bp-MRI protocols had an equal detection rate of high-grade PCa to mp-MRI. “Fast” bp-MRI can double prostate MRI capacity at lower expenses. This is, however, at the cost of 2% more biopsies and 1% more overdetection of low-grade PCa.
Written by: Marloes van der Leest, MD,1 Bas Israël, MD, MSc,1,2 and Jelle Barentsz, MD, PhD1
Author Affiliations:
1. Department of Radiology and Nuclear Medicine, Radboud University Medical Center, Nijmegen, The Netherlands
2. Department of Urology, Radboud University Medical Center, Nijmegen, The Netherlands
References:
1. van der Leest M, Cornel E, Israel B, et al. Head-to-head Comparison of Transrectal Ultrasound-guided Prostate Biopsy Versus Multiparametric Prostate Resonance Imaging with Subsequent Magnetic Resonance-guided Biopsy in Biopsy-naive Men with Elevated Prostate-specific Antigen: A Large Prospective Multicenter Clinical Study. Eur Urol. 2019;75(4):570-578.
2. Drost FH, Osses DF, Nieboer D, et al. Prostate MRI, with or without MRI-targeted biopsy, and systematic biopsy for detecting prostate cancer. Cochrane Database Syst Rev. 2019;4:CD012663.
3. Kasivisvanathan V, Stabile A, Neves JB, et al. Magnetic Resonance Imaging-targeted Biopsy Versus Systematic Biopsy in the Detection of Prostate Cancer: A Systematic Review and Meta-analysis. Eur Urol. 2019.
4. van der Leest M, Israel B, Cornel EB, et al. High Diagnostic Performance of Short Magnetic Resonance Imaging Protocols for Prostate Cancer Detection in Biopsy-naive Men: The Next Step in Magnetic Resonance Imaging Accessibility. Eur Urol. 2019.
Read the Abstract


