Benefits of adjuvant IO therapy include:
1) Prevention of getting stage 4 metastatic disease
2) Possibly shorter duration of treatment (1 year vs. 2 years in metastatic setting)
3) Possible “better” immune system as patients are usually healthier and more robust
4) Normal LDG or good performance status
However, on the contrary, because they are healthier, to begin with – they may have more side effects and a portion may get unnecessary treatment.
He focused a bit on the melanoma situation with Stage 3 tumors – multiple recent studies have suggested RFS benefit in stage III disease. But the benefit varies from stage 3a to stage 3d disease – and weighing the risks/benefits at each stage is important, and is very patient-specific.
His open questions for adjuvant IO therapy are:
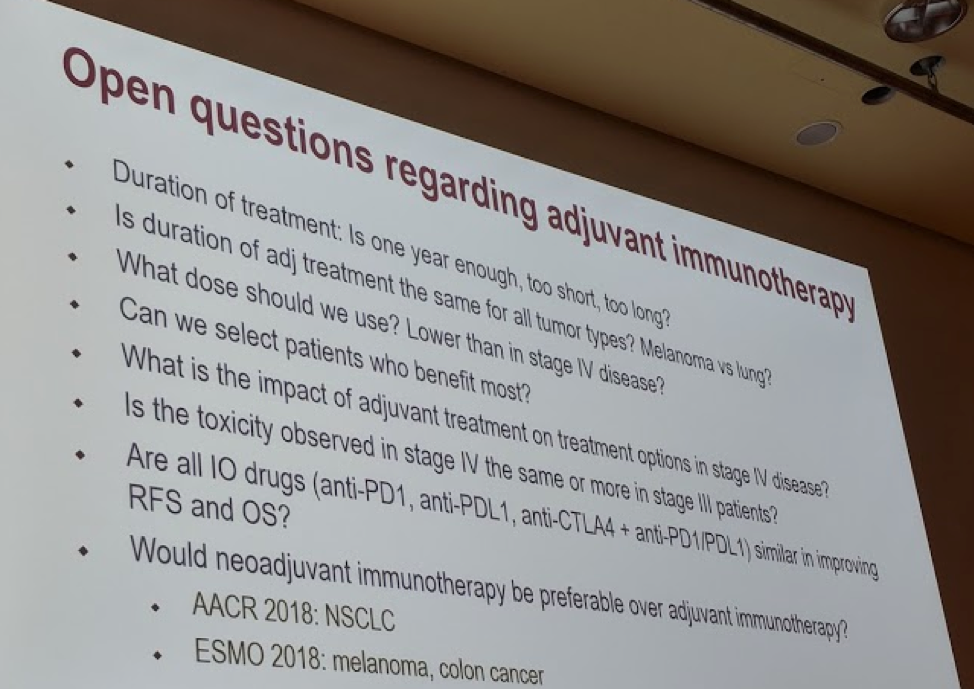
These are yet unanswered in all disease states, and further work is needed.
Presented by: John B. Haanen, MD, Head of the Division of Medical Oncology and Staff Scientist in the Division of Immunology, Professor of Translational Immunotherapy of Cancer at Leiden University Medical Centre, Amsterdam, the Netherlands
Written by: Thenappan Chandrasekar, MD, Clinical Instructor, Thomas Jefferson University, twitter: @tchandra_uromd, @TjuUrology at the 2018 European Society for Medical Oncology Congress (#ESMO18), October 19-23, 2018, Munich Germany


