This combination of enhanced tumor seeding and impaired immune response may increase the susceptibility of patients undergoing surgery to the development of future metastases. Recently, Hong et al. studied the long-term oncologic outcomes of volatile inhaled anesthesia (VIA) and total intravenous anesthesia (TIVA) and concluded that differences in tumor recurrence and overall survival depended on cancer type.6 Additionally, Orriach et al. analyzed this difference in patients who underwent robot-assisted radical cystectomy (RARC) for bladder cancer and found that patients who received propofol and local anesthesia had longer disease-free survival compared to those who received sevoflurane and opioids (585 vs. 210 days; p=0.01).7
In an effort to address this point, we investigated whether there is a difference in distant recurrence between the use of TIVA or VIA in patients who underwent RARC.
Using our institutional database of all patients who underwent RARC for muscle-invasive or high-risk non-muscle-invasive bladder cancer from 2014 to 2020 we investigated the association between anesthesia and cancer recurrence. The primary endpoint of our study was distant recurrence-free survival, which was defined as the length of time between the date of RARC and the date of the first scan showing distant recurrence. Recurrence of bladder cancer was determined as local or distant, and confirmed by radiologic or histologic examination. For our analyses, only patients who experienced distant recurrence were included. Distant recurrence was defined as any recurrence excluding those in the urethra, ureter, or renal pelvis.
Briefly, we identified 231 patients who underwent RARC at our institution. Of these, 126 (55%) received TIVA and 105 (45%) received VIA, there were no differences in tumor and patient characteristics between these two groups. Distant recurrence occurred in 8.7% and 26.7% of patients who received TIVA and VIA, respectively (p<0.001). Kaplan Meier analysis demonstrated a significant improvement in distant recurrence-free survival with the use of TIVA (log-rank p<0.001) (Figure 1). Multivariable analysis revealed a significant increase in recurrence risk with VIA (hazard ratio [HR]: 3.4, 95% confidence interval [CI]: 1.5-7.7, p<0.01) and increase tumor pathological stage (pT2, pT3, pT4, all p<0.05).
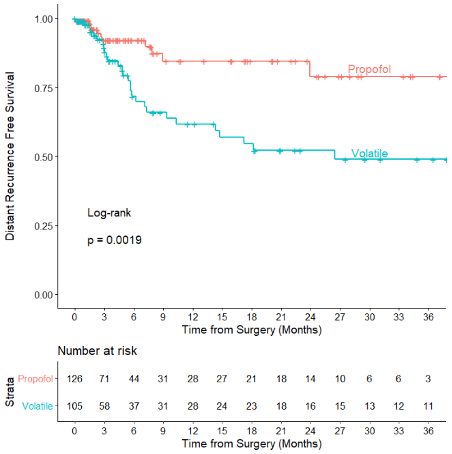
Figure 1. Kaplan Meier analysis of distant recurrence-free survival stratified by anesthetic received.
From these data, we found that patients who received VIA were at a significantly greater risk for developing distant recurrence compared to those who received TIVA. We feel that this information has several important implications: first, these preliminary results can serve as a hypothesis-generating study for future analyses. Second, these results may be used during perioperative planning in order to improve long-term oncologic outcomes.
According to our study, among all patients who underwent RARC at our institution, those who received total intravenous anesthesia experienced a significant improvement in distant recurrence-free survival compared to those who received volatile inhalation anesthesia 8. These data emphasize the importance of prospective studies aimed at analyzing the effect of anesthetic technique on long-term oncologic outcomes. One such study, GA-CARES (NCT03034096), is currently underway.
Written by: John L. Pfail, and John P. Sfakianos, MD, Department of Urology, Icahn School of Medicine at Mount Sinai, New York, New York
References:
- Siegel, Rebecca L., Kimberly D. Miller, and Ahmedin Jemal. "Cancer statistics, 2020." CA: a cancer journal for clinicians (2020). 70, 7-30.
- Chang, Sam S., Bernard H. Bochner, Roger Chou, Robert Dreicer, Ashish M. Kamat, Seth P. Lerner, Yair Lotan et al. "Treatment of non-metastatic muscle-invasive bladder cancer: AUA/ASCO/ASTRO/SUO guideline." The Journal of urology 198, no. 3 (2017): 552-559.
- Chang, Sam S., Stephen A. Boorjian, Roger Chou, Peter E. Clark, Siamak Daneshmand, Badrinath R. Konety, Raj Pruthi et al. "Diagnosis and treatment of non-muscle invasive bladder cancer: AUA/SUO guideline." The Journal of urology 196, no. 4 (2016): 1021-1029.
- Tohme, Samer, Richard L. Simmons, and Allan Tsung. "Surgery for cancer: a trigger for metastases." Cancer research 77, no. 7 (2017): 1548-1552.
- Stein, John P., Gary Lieskovsky, Richard Cote, Susan Groshen, An-Chen Feng, Stuart Boyd, Eila Skinner et al. "Radical cystectomy in the treatment of invasive bladder cancer: long-term results in 1,054 patients." Journal of clinical oncology 19, no. 3 (2001): 666-675.
- Hong, Boohwi, Sunyeul Lee, Yeojung Kim, Minhee Lee, Ann Misun Youn, Hyun Rhim, Seok-Hwan Hong, Yoon-Hee Kim, Seok-Hwa Yoon, and Chaeseong Lim. "Anesthetics and long-term survival after cancer surgery—total intravenous versus volatile anesthesia: a retrospective study." BMC anesthesiology 19, no. 1 (2019): 233.
- Orriach, Jose Luis Guerrero, Aida Raigon Ponferrada, Alfredo Malo Manso, Bernardo Herrera Imbroda, Juan Jose Escalona Belmonte, Marta Ramirez Aliaga, Alicia Ramirez Fernandez et al. "Anesthesia in Combination with Propofol Increases Disease-Free Survival in Bladder Cancer Patients Who Undergo Radical Tumor Cystectomy as Compared to Inhalational Anesthetics and Opiate-Based Analgesia." Oncology 98, no. 3 (2020): 161-167.
- Pfail, John L., Andrew B. Katims, Zeynep Gul, Shoshana J. Rosenzweig, Shirin Razdan, Sarah Nathaniel, Alberto Martini et al. "Can anesthetics affect bladder cancer recurrence? Total intravenous versus volatile anesthesia in patients undergoing robot-assisted radical cystectomy: A single institution retrospective analysis." In Urologic Oncology: Seminars and Original Investigations. Elsevier, 2020.


