In our paper, we highlight a previously unreported clinical finding in a patient with urothelial bladder cancer metastatic to the peritoneum who was treated with anti-PD1 immunotherapy. Notably, the patient developed recurrent large-volume ascites. While this finding is typically highly concerning for disease progression, this patient was found to have a significant reduction in size of peritoneal nodules on imaging, and no malignant cells could be recovered from the fluid upon repeated paracenteses.
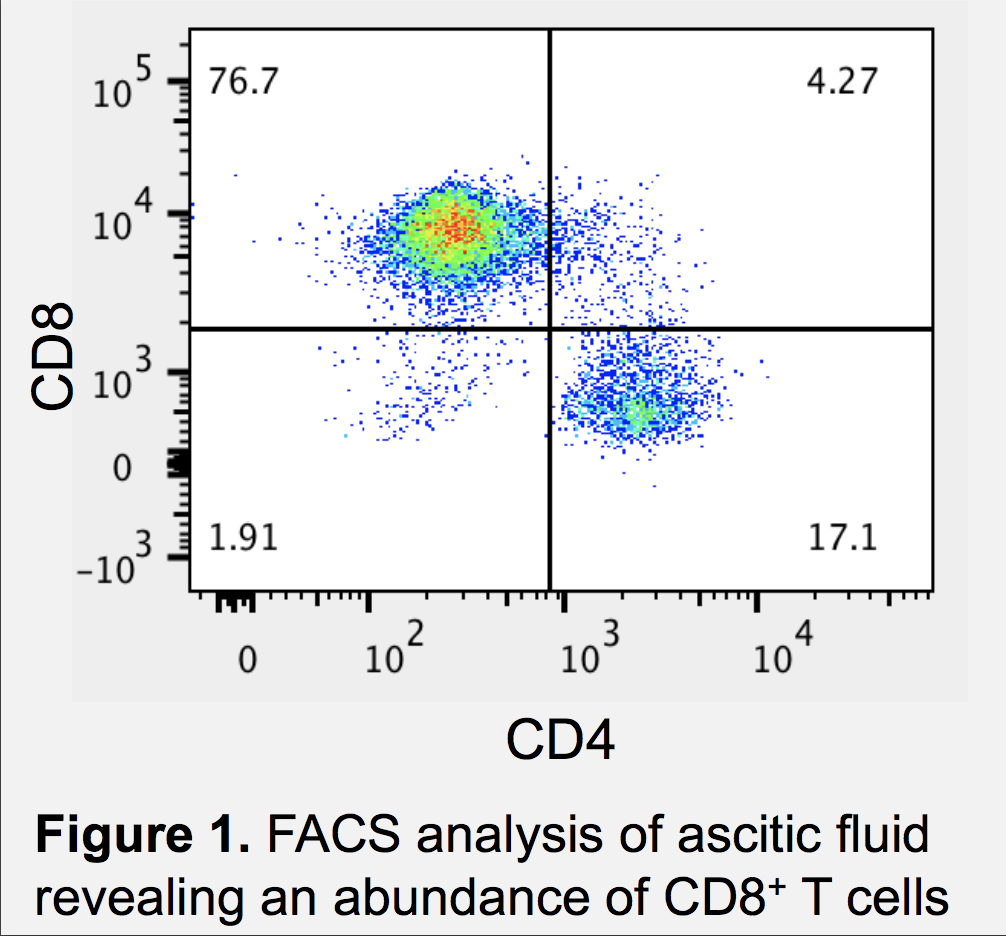
Immune checkpoint blockade is now the standard-of-care multiple genitourinary malignancies, and radiographic pseudoprogression has emerged as a real, albeit rare, phenomenon. Emerging literature, including this report, indicate that clinical pseudoprogression is another important phenomenon that occurs when manifestations typical of clinical progression occur in the context of a patient having an anti-tumor immune response. With both radiographic and clinical pseudoprogression, the findings are caused by rapid proliferation of activated T lymphocytes. In this study, flow cytometry revealed a high proportion of activated CD8+ T lymphocytes based on surface markers (Figure 1), and cytokine analysis indicated high levels of IL-6 and IL-15. In summary, ascites during immune checkpoint therapy, particularly in the setting of peritoneal metastases, can result from T cell expansion. Pseudoprogression is rare, so clinical judgement remains paramount in deciding a course of action.
Written by: Randy F. Sweis, M.D. Department of Medicine, Section of Hematology/Oncology, Comprehensive Cancer Center, University of Chicago Medicine, Chicago, IL
Read the Abstract


