Contents
- Overactive Bladder Symptoms
- Patient History & Situation
- Severity of Urine Leakage
- PTNS Treatment
- Nerves Affected
- Insurance & Medical Necessity
- Preparing the Patient
- Flexion Response
- Treatment Results
- Summary
Introduction
Welcome. I'd like to present a case study on refractory overactive bladder with severe urinary incontinence by using percutaneous tibial nerve stimulation or PTNS.
I am Diane Newman. I'm a nurse practitioner and the adjunct associate professor of urology and surgery, research investigator senior at the Perelman School of Medicine and the University of Pennsylvania. I also co-direct the Penn Center for Continence and Pelvic Health within urology at the University of Pennsylvania in Philadelphia.
I've been doing PTNS now for over 18 months and I want to share with you a really interesting case study that I hope that you will find is fascinating as I do.
Overactive Bladder Symptoms
This was a woman 64 years of age who had a greater than five year history of urgency, frequency, and urgency urinary incontinence. She reported that she urinates greater than 14 times during the daytime. Notcuria doesn't seem to be a problem. It may be once, but usually may be zero.
Her incontinence occurs primarily after urgency and she uses three large ultra, so the bigger ones, perineal pads. And additionally she puts tissue in the pads for added protection. At our practice, we use the AUA symptom score as a questionnaire for low urinary tract symptoms and she recorded that it was a 10 with her urinary symptoms being terrible. So that's how she described her symptoms.
Patient History & Situation
She's had five pregnancy, four vaginal deliveries. Her BMI, it would be classified as obese. She has high blood pressure, osteoarthritis, and seven years ago she underwent a hysterectomy. Many of my patients of this age group I do get after undergoing some type of pelvic surgery, usually hysterectomy, when they start to notice worsening of symptoms.
She is also post-menopausal. So again, she's a typical patient that I would see coming in.
Now, I think why her symptoms, she feels, are very severe is that she works as a teacher and she was really upset about the fact that throughout the day all she does is worry about urine leakage, which is why she's wearing the pads, plush additional tissues. She doesn't want to wear protective underwear. She finds him too bulky and she was concerned that you'd see them underneath her pants, which she wears at work.
But she's very concerned and very anxious about possibly saturating through pads while at work. Frequency really is only a bother and an issue while at work. If she's home on the weekends, it's not as much of an issue. And she states that she does go to the bathroom more frequently when she's anxious and she feels she's anxious all the time.
She has urgency, but that didn't appear to be as much of an issue with her.
Types of Incontinence
Want to share with you some information on the different types of incontinence because I think that when we look at treating patients with refractory overactive bladder with PTNS, we want to really look at what is their most bothersome symptom.
Premenopausal
As you can see in women premenopausal, stress incontinence tends to be the most prevalent type of incontinence. With mixed not far behind.
Older Patient
But with aging starting 65 years and then 80 plus, you see that the mixed symptoms are more predominant.
And in this patient you see that stress, urge, and mix are almost the same. So a lot of them do come in with mixed incontinence. And this was done ... This is an NIH evidence report technology out of the NIH several years ago.
Severity of Urine Leakage
I think as clinicians we have a very difficult time quantifying UI severity. This patient, AUA symptom score was 10, which is in the moderate range. However, she feels her symptoms are very severe. They're very severe to her because she can't function at work.
They're severe and there's really no data on what is the different levels as far as severity of urinary leakage. This is something I put together for my publication, "Managing and Treating Urinary Incontinence," to try to quantify it in the amount of quantity of urine leakage.
Quantifying Urinary Incontinence
Such as:
- A small volume is less than 30. It's enough to make underwear wet.
- Moderate volume is more than that, up to three ounces. It's enough to have wet or soak underwear and may leak out of the underwear down the legs.
- Large volume is 100 plus MLs. It soaks through clothing and onto floor. So it's usually the whole entire bladder volume.
Sandvik Questionnaire Research
There's a very recent publication, May of this year that looked at the prevalence of severe urinary incontinence in the nurses' health study that's been going on for many, many years. And I found this of interest because it's one the most recent studies that looked at severity of incontinence.
So I really suggest that you look at this study because it might provide you with some additional information that might help you as you see patients like the one I'm presenting today in this webcast. But this is a large number. Look at that. 150,000+ women and they quantified by using the Sandvik questionnaire.
"During the past 12 months, how often have you leaked or lost control of your urine?" And then they quantified less than once a month, two to three times per month, once per week, or once per day. And when you lose urine, how much? Now, they only quantified a few drops or more than drops. So a few drops of slight or mild, and then more.
And again, they use the Sandvik Severity Index, which was published many years ago. And many of us use it in research. And frequency of UI is assigned a value from one to four. Higher number, of course in the case of greater frequency and the amount of leakage assigned a value of one equals drops or more and two for more than drops.
And you can see where they ... With severity, they combined frequency plus the amount of leakage. So, how often they had these UI episodes and then the quantity, how much. So I think it's an interesting way to quantify the severity of incontinence and their data is really, I think fascinating.
They broke it down in these year ranges, which I think is important. So from 41 up to 83. and as you can see, there's not a lot of variation as far as quantity of urine loss. It's about a a good fourth and again, large number of women, over 100 thousand.
And you can see of course the largest number actually was right about the age group of ... The case study I'm talking about today with 31,000 women and they had about a 22% severity. Whereas, the largest number who reported the largest amount of severity is those older adults.
So this might be of interest to you. Look at the whole article because it does break down other levels of urinary incontinence.
But I think that what I find in practice, and I think many of you probably listening to this will agree, is that severity in impact on quality of life is subjective and depends on an individual patient. I often listen to a patient report their symptoms and think about, "Well, that's not as bad as what I see, say, in other patients." And then they're devastated by it, they cannot manage it, they don't want to go out of their house.
So it really is subjective and I think that we have to be cognizant of that as clinicians because patients ... That does lead to disappointment with outcomes, but also leads to sometimes unrealistic expectations of treatment.
Now, as I said before, we use the AUA symptom score and as you can see what's ... And many urology offices use this as a questionnaire of low urinary track symptoms, but it doesn't cover incontinence. So it's not surprising to know that this woman's score was 10, which is moderate, but she felt her urinary symptoms are terrible.
And I love this question down here because it kind of orients me to where I am with that patient as far as bother. So even though it was a score which is moderate, she felt her symptoms were just terrible. And I used this as I had her undergo PTNS with a bladder diary. I really did track this to see if her symptom score had improved.
PTNS Treatment
Now I'm sure by looking at the website you see a lot of information on PTNS, it is for refractory overactive bladder. I did try conservative treatments on this patient. She went over a very aggressive behavioral treatment program as well as medications.
Actually, when she first came to me she wanted medications. She didn't want anything else. She was looking for a fix that would help her in the school hours next week, so she wanted something immediate. So she did try several antimuscarinics with only moderate success, but she didn't really ... She did some improvement with conservative therapy, but not enough and she continued to have bothersome symptoms.
This is out of actually the article looking at the treatment algorithm and you can also find this in the AUA guidelines
Nerves Affected
Now, PTNS for you who are not familiar with it, it's called UrgentⓇ PC system. It requires a unit that's a nine volt battery, delivers 200 milliseconds of pulse. It activates flexion of the great toe or fanning of the toes, two to five.
This is a grounding pad that is a medial surface calcaneus right there and typically 12 weeks, 30 minute sessions. You use a 34 gauge needle, it's placed three to four sonometers above the medial malleolus and the medial aspect of the fibula.
In this webcast, I'm going to go through some really specifics on how you prepare patients for this treatment. And basically the posterior tibial nerve is put in this area here, the tibial nerve branches off the sciatic nerve L4 to S3 nerve roots, and it provides innovation to posterior leg, foot and cause plantar flexion.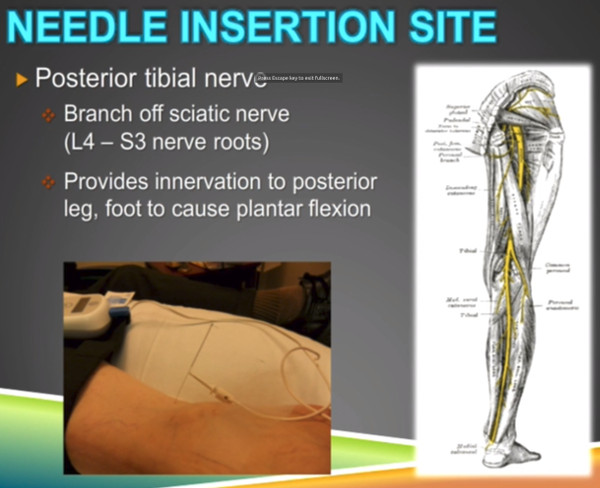
In the foot it fans out the tibial nerve and I actually use this picture on my patient education handout and I try to print it out in color so the patient sees it. You know, "What do you mean you put a needle in my ankle? How's that going to affect my bladder? Which is, as you told me, up here in my pelvis."
Well the fact that the tibial nerve innovates this sacral area in how it travels down the leg there. So I think that's a very helpful picture.
Medical Necessity
Completing medical necessity is very necessary. Where I practice, I do not get approval for insurance coverage of PTNS unless I do complete the medical necessity form. Now, I want to point out some important things related to this case study. Severity, she considered a five. It disrupting her life, and it was. She had a hard time teaching and this was her career contraindications.
Contraindications, that's very important to look at. In this one she only had really no contraindications. That's actually an error, she did not have diabetes. And patient goals. I asked them what do they want to change. I always ask this up front.
She wanted decreased frequency and she definitely wanted less incontinence. This form is completed and it actually goes to the insurer with my notes and they will only approve it if they of course failed behavioral and antimuscarinic therapy.
Preparing the Patient
Now the setup, I always have the patient complete a diary at baseline to try to see where her symptoms are before I start the treatment. Check that unit battery for adequate charge. I have forgotten this a couple times and it stops in the middle of the treatment. You don't want that to happen.
You want the patient to sit comfortably here. This is an arm chair. I actually have them sit on our exam table with the leg up. They should remove of course ... They should remove the shoe and stockings. You should elevate the leg.
I try to support it and I also support the other leg because I've had a couple of times where this has fallen. The unit has fallen and pulled a needle out of the leg. So you want to support it so it does not move. And I tell the patient, "Please don't move your leg throughout the treatment." But I want them comfortable.
My patients will either bring an iPod to listen to music. Some bring a book, some bring an iPad to read a book, or they'll read the newspaper for that day that we have in the office.
And if they want to take a nap, I actually turn on the little light that's over our sink and I turn off the big lights in the exam room and they can take a 30 minute nap. So whatever works for you and the patient.
Type of Needle, Insertion Point, Grounding Pad
As I said before, you want to hit this area. So you want that foot turned outward so you can really identify the medial malleolus for the tibial nerve insertion.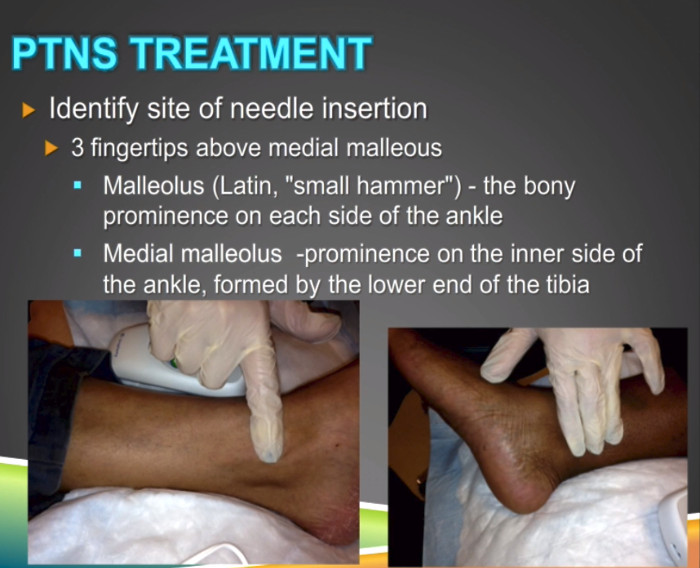
You want to identify, and it's usually three fingertips above that. And malleolus means small hammer in Latin. And if you feel that bone there, that's what it feels like. It's a little bit of a hammer. It's a bony prominence on each side of the ankle.
So you want that ankle turn outward, you want to feel that with your finger, and as you see here it's three fingertips above it. Okay? And that's usually the marker. So I would put the needle right below that.
And this is really inserting the needle. I'm in this case, what I did was I left my fingers there and put the needle right below and I inserted very, very gently. And I have not had ... I've had a few cases where it has been painful.
I actually just recently last week had a case where I put the needle in each ankle and she couldn't tolerate it, so I didn't do the treatment. But that's very, very rare. Usually they don't feel it as it's inserted in. It's a very thin needle and I show it to patients. It's similar to an acupuncture needle.
You want to put the grounding pad on the calcaneus right here, and if you wipe that area before putting the pad on it would adhere better. I found out on my own that the unit will not function if the grounding pad is not placed. So that's very, very important. All right?
Now as I said before, you want to support the unit to prevent displacement during treatment. Here I've taped the electrode wire to keep the needle stable. You can do that if you want. It's up to you, but you see I put them on pillows here. That's very typically what I do as far as supporting the leg.
Flexion Response
Now, response. I want to show you some really great responses that I got with my patients. Flexion, you want to see toe flexion and flexion is bending the joint, resulting in a decrease of angle. And as you can see, this patient has a fantastic flexion and this happens every time. She even sees it.
So this is no flexion and with the stimulation you can see that toe really flexing down. So this is a very significant response for flexion. This is also the case with this. Actually, this toe just kind of a flexed up and it really was very different than prior to starting the stimulation.
Now I get asked by a lot of clinicians, "Well, what if I don't see toe flexion?" Well, you've got to remember that the posterior tibial nerve is a mixed sensory motor nerve. So either sensation or motor response may indicate correct placement.
So in some patients I don't get flexion, but I do get a sensation response. So patients will experience sensation like tingling or tapping on the sole or heel of the foot. I usually find that it travels.
They will tell me that, "Oh, it's starting. It's by the needle, now it's traveling down into my heel. Oh, yeah. I feel it in my toe." So it does usually travel, but it may just stay at the ball of the foot and that's still fine. So it may just sensation.
How many patients I get toe flexion? I don't know, maybe 40% and maybe 60% I get sensation or ... No. Probably about 30% I get sensation and probably the rest I get toe flexion and sensation. A combination. So if you don't get toe flexion, don't be worried. The patient should feel the sensation of that stimulation though.
By the way, some things that may alter that is if the patient has edema they may not feel it. If there's a lot of fat in that ankle, you may not be getting to the tibial nerve. So those patients I've had some issues with.
Treatment Results
Now I want to show you her kind of whole visit and then she's now had two boosters. I do give monthly boosters in certain patients who start to see improvement. As you can see here, she started out, like I said, AUA symptom score was 10. It was terrible, she quantified her symptoms.
Frequency was 14, she was using in large perineal pads with tissue. Some of her frequency, by the way she poured was the fact that she thought if she kept her bladder empty she wouldn't have to go, so she wouldn't have incontinence. And you hear that all the time from patients.
And as you can see for the first five/six visits, really no change here. And I don't have them do bladder diaries each visit. You can see here I had them do them every other and then I did a few more at the end. And I usually don't see improvement until about the sixth treatment, I tell patients.
So here she stopped. She thought she may be using less tissue here, she said she was. Here, she went to two to three frequency. Has decreased nicely. You see that. By visit 11 she had switched to a less absorbent pad and now you see the change in the AUA symptom score where she's mixed equally. Satisfied that the number was nine.
By the end of treatment she was down to two medium pads. So she dropped down from that large super absorbent pad down to medium, frequency was 10. I didn't have her do the symptom score here. And then as she's coming back you see it's decreasing even further.
I'm sorry, that should be nine to 10. that six is an error. But the point is, is that now she's mostly satisfied and here she says she's pleased. So you can see that nice progression.
Now this is over 12 visits, plus another two months. So you can see that it takes some time. We're talking about over almost a six month period and that may happen. And I tell patients, you do not expect improvement right away. You really need to set up expectations with this.
Summary
So I have found PTNS to be very successful in my patients with refractory overactive bladder who have failed drug therapy and a very comprehensive behavioral treatment program.
I do still have patients on some. Some of my patients are on PTNS, maybe on a small dose of antimuscarinic. But by the end of the treatment I do have them stop the med to see what happens. Some of them do continue on some of the exercises, the urge training, but most have failed it.
It is a minimally invasive 30 minutes treatment in-office. It can be done by an MD, NPRN or PA. 12 treatments typically once a week, but now it's the holidays. So I do have patients who have skipped the Thanksgiving week and I'm sure I'm going to have more that will skip Christmas week.
Symptom improvement may not be seen until the second half of the treatment. So after that sixth treatment I tell patients that. Don't expect improvement right away. And I really like that three-day bladder diary to monitor symptoms. And actually, that supports medical necessity for insurance. So I have patients do it throughout the treatment.
I also have them do that AUA symptom score. Not maybe as often as I've showed you in this case study, but I do have them do it baseline mid treatment and then at the end to see if we see improvement.
So I hope this case study was helpful and hopefully you would share some of your stories and your patients with us. I think that would be really helpful for our audience. Thank you.


