Berg et al provided a thoughtful review of how telehealth can be incorporated into male infertility practices.2 We build on this practical description focused on logistics and implementation by providing data on the conditions that have been previously managed through video visits, the safety of providing virtual care, and benefits to patients through cost and travel savings.
Findings:
- Between August 2017 and March 2020, 70 male infertility video visits were completed by 56 different men.
- There was a broad array of male infertility diagnostic categories observed during video visits, including endocrinologic conditions (29%); anatomic causes of infertility (27%); idiopathic infertility (16%); concerns regarding medical treatments on fertility potential (9%); partners being evaluated by REI (9%); genetic abnormalities (7%); and low DNA integrity (3%).
- Video visit patients received a variety of interventions - Figure 1

- In the 90 days after video visits, there were only two in-person encounters (3%) within our health system, both of which were planned post-operative visits after varicocelectomy. No patients required an unplanned office or emergency department visit in the three-month period after their telehealth follow-up.
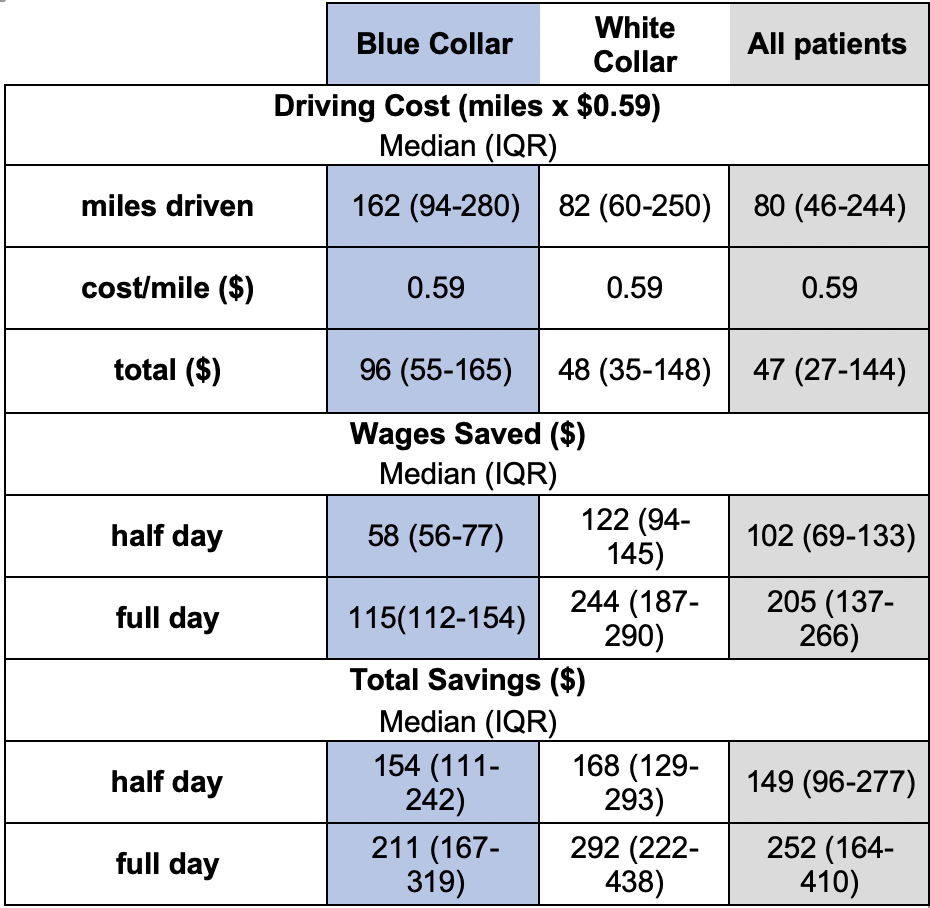
- Video visits eliminated driving time and travel-related costs as well potentially preventing lost wages by reducing time off work.
Together, these findings suggest that video visits can serve as practical substitutes for an in-person visit for infertility care if a physical exam or in-office procedure is not needed at the follow-up appointment. The cost and travel savings are consistent with data across other institutions and urologic conditions highlighted by the American Urological Association Telehealth White Paper.3
It remains to be seen what telehealth regulation and reimbursement will look like beyond the COVID-19 public health emergency; however, virtual care gives patients another option for where and how they can access specialty care.
Written by: Juan Andino, MD, & James M. Dupree, MD, The University of Michigan Health System
Written by: Juan Andino, MD, & James M. Dupree, MD, The University of Michigan Health System
References:
- Adam J. Gadzinski, MD, MS, Chad Ellimoottil, MD, MS, Anobel Y. Odisho, MD, MPH, Kara L. Watts, MD, John L. Gore, MD M. Telemedicine in urology: A crash course during the COVID-19 pandemic. Urology Times. 2020. 48, 4, 48, 04.
- Berg WT, Goldstein M, Melnick AP, Rosenwaks Z. Clinical implications of telemedicine for providers and patients. Fertil Steril. 2020 Dec;114(6):1129-1134.
- Gettman M, Rhee E, Spitz A. Telemedicine in Urology. American Urology Association. Published 2016, Amended 2021.
Read the Abstract


