BERKELEY, CA (UroToday.com) - In the past decades open pyeloplasty has been the gold standard for treating ureteropelvic junction obstruction with a high success and low complication rate. However, minimal invasive surgery has now become an alternative treatment with comparable short- to intermediate-term success rates and the benefits of postoperative decreased pain, shorter hospitalization, rapid convalescence, and an improved cosmetic result. For the minimal invasive approaches, specifically, classical laparoscopy vs robot-assisted laparoscopy, these benefits must be balanced against the increased costs of the robotic platform. Compared with the laparoscopic approach, robotic-assisted is known to facilitate intracorporal suturing. To date, only few studies have published data concerning long-term results of robot-assisted pyeloplasty (RAP) in adults.
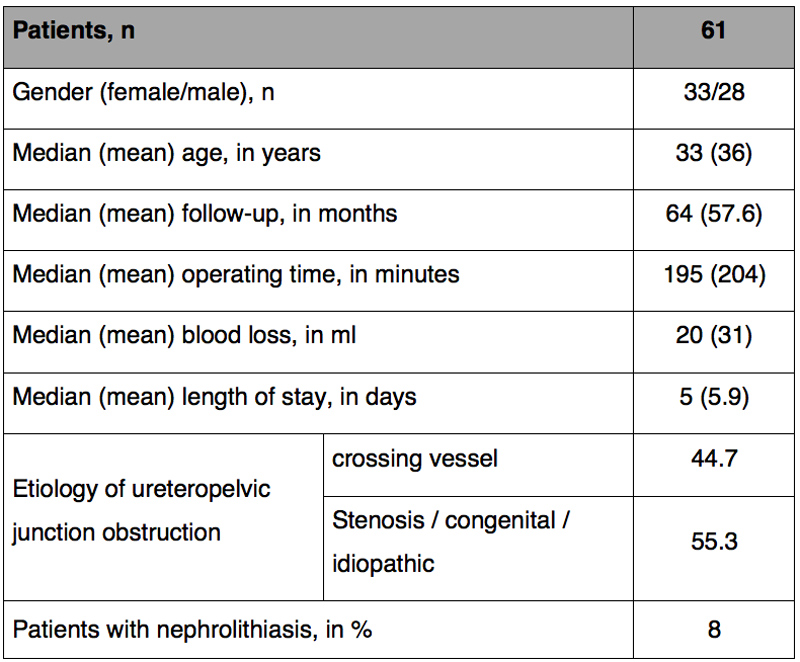 |
| Table 1: Patient characteristics and intraoperative findings |
We retrospectively reviewed our RAP experience of 61 patients performed by two surgeons between 2004 and 2013 regarding operating time, length of hospital stay, perioperative complication, and success. Median follow-up was 64 months; more than 80% of patients had a follow-up of over 2 years. Patients characteristics are shown in table 1.
Overall success was measured on necessary redo pyeloplasty. We also identified patients with temporary stent placement due to symptomatic hydronephrosis, or with further obstruction in diuretic renography.
In all 61 patients, a dismembered Anderson-Hynes pyeloplasty with transperitoneal approach was performed with antegrade ureteral stent placing. The ureteral stent was removed after a minimum of 4 weeks. The majority of patients had a control diuretic renography 2-4 weeks after stent removal for evaluating the obstruction as well as ultrasound to control the degree of residual dilatation. For long-time follow-up we contacted patients and treating urologist to ask for recurrent symptoms with temporary stent placement or re-do pyeloplasty. No conversion to open procedure was necessary. The success rate was 98% (n=60) with one patient undergoing open redo pyeloplasty due to a recurrent stenosis. Temporary stent placement was reported in 3 patients due to pyelonephritis and dilatation.
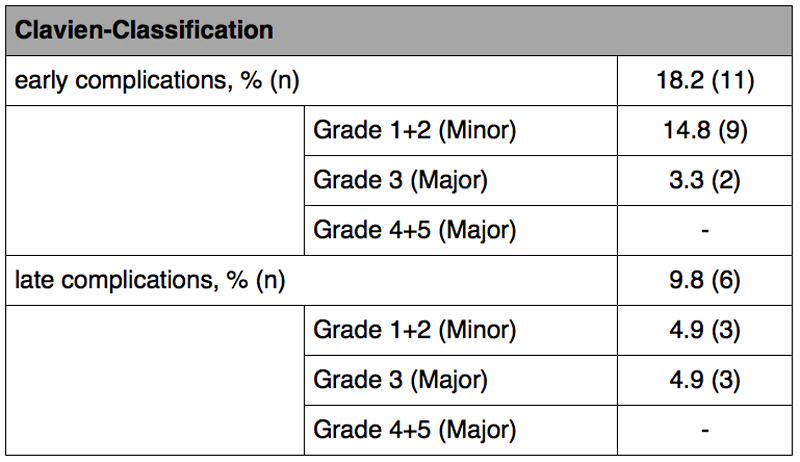 |
| Table 2: Complication rates |
Table 2 shows postoperative complication rates. Overall we reported early minor complications such as urinary tract infections, prolonged drainage, and bowel paralysis in 18.2% of patients (n=11). Major complications occurred in two patients (3.3%): trocar bleeding and insufficiency of the anastomosis with necessary re-do anastomosis. Late major complications included patients with symptomatic hydronephrosis who needed temporary stent placement. 77% of patients (n-47) were free of any complications, major complications grade > 4 did not occur.
Overall we could demonstrate that robotic-assisted pyeloplasty is not only a feasible and safe, but more importantly, in long-term follow-up, RAP represents an effective technique for treating ureteropelvic junction obstruction.
Written by:
Miriam Traumann as part of Beyond the Abstract on UroToday.com. This initiative offers a method of publishing for the professional urology community. Authors are given an opportunity to expand on the circumstances, limitations etc... of their research by referencing the published abstract.
University Medical Center Hamburg-Eppendorf, Department of Urology, Hamburg, Germany


