Dr. Meagan Dunne and her colleagues sought to report the surgical outcomes of 10 patients on anticoagulation who underwent mini-PCNL and to determine if mini-PCNL is feasible for these patients. These 10 patients had their surgeries performed between 2018 and 2019. All operations were performed by 2 surgeons in a hospital setting. Tract size was 17Fr and renal access was obtained by the operating surgeon. Patients were on apixaban, rivaroxaban, warfarin, or clopidogrel. No intraoperative complications related to bleeding were noted and no patients required blood transfusions. On postoperative day 1, there was a mean hemoglobin change of 1.24g/dl. One patient had a small hematoma on postoperative day 1.
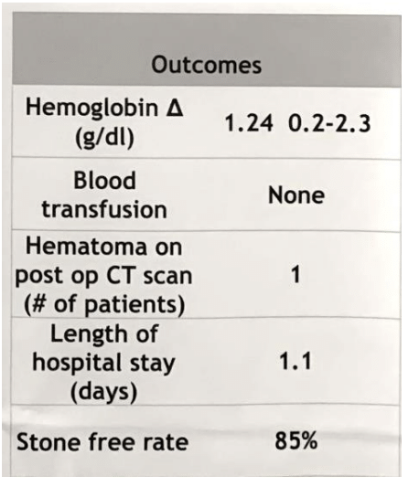
In conclusion, mini-PCNL can be cautiously considered in select high-risk patients on full anticoagulation.
Presented by: Meagan M. Dunne, MD, University of Maryland Medical Center, Chesapeake Urology and University of Maryland BWMC
Written by: Lillian Xie, BA, Department of Urology, University of California, Irvine, California, at the 37th World Congress of Endourology (WCE) – October 29th-November 2nd, Abu Dhabi, United Arab Emirates


