(UroToday.com) The 2023 Society of Urologic Oncology (SUO) annual meeting held in Washington, D.C. between November 28th and December 1st, 2023, was host to the Confederación Americana de Urología (CAU) session. Dr. Lara Rodríguez Sánchez presented the Falcon Project which aims to reach a consensus on focal therapy usage in prostate cancer patients.
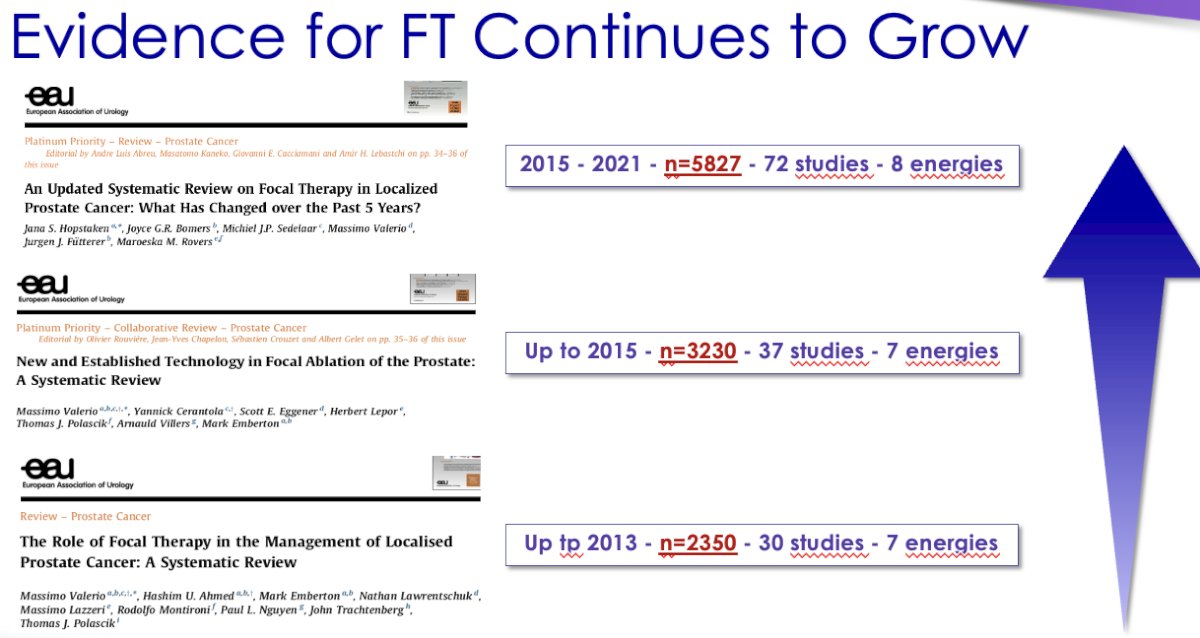
Dr. Rodríguez Sánchez began by noting that focal therapy for prostate cancer is an interactive technological approach focused on consolidating a personalized, effective, and less aggressive treatment for prostate cancer. The major current limitation is that, although improved functional outcomes have been proven, long-term oncological results are awaited, and there is no final consensus on the implementation of focal therapy. However, it is clear that the evidence for focal therapy continues to grow:
But focal therapy is already here, and Dr. Rodriguez Sánchez noted that we need to bring some ‘order’ to all of this. That's why consensus is important. Falcon is not the first consensus; at least ten others have been published before. However, previously available consensuses were limited to those including experts' opinions on focal therapy only. With Falcon, there is an attempt to carry out a broad international consensus on focal therapy, including all those who can be part of one of their tumor committees – not necessarily just experts who perform the technique and may provide a biased view strongly in favor of this approach.
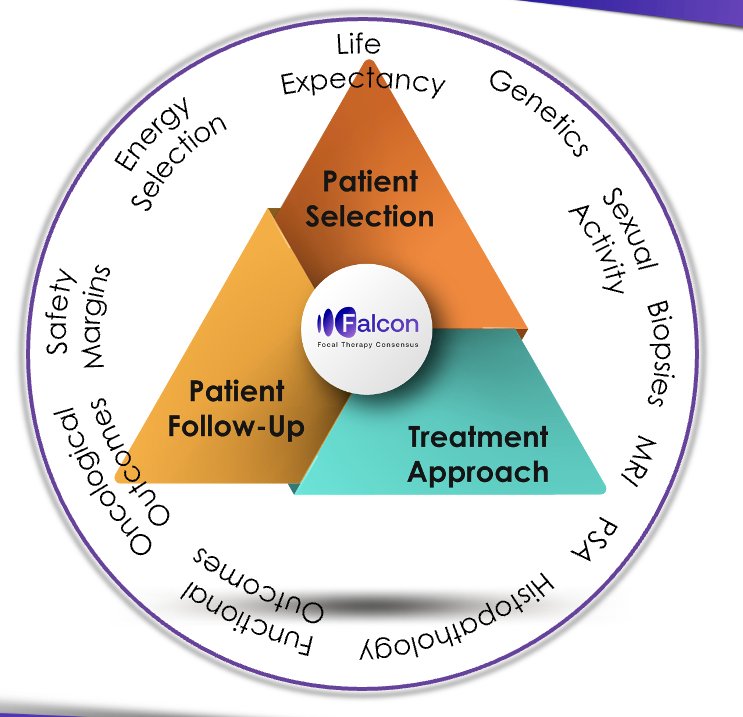
After an expert meeting and a narrative review, the investigators identified all the points of conflict related to focal therapy. These include those related to patient selection, patient follow-up, and treatment approach.
The investigators conducted three rounds of a Delphi Consensus with the assistance of the DelphiManager software supported by the University of Liverpool. Participants were invited to score their agreement with every statement on a 1 – 9 Likert scale, with an 'unable to rate' option available. All statements that reached consensus during the second round were removed for the third round. The threshold for consensus was set at a minimum of 70% of the number of respondents. In the final stage, a final face-to-face expert meeting was conducted (October 12th, 2023).
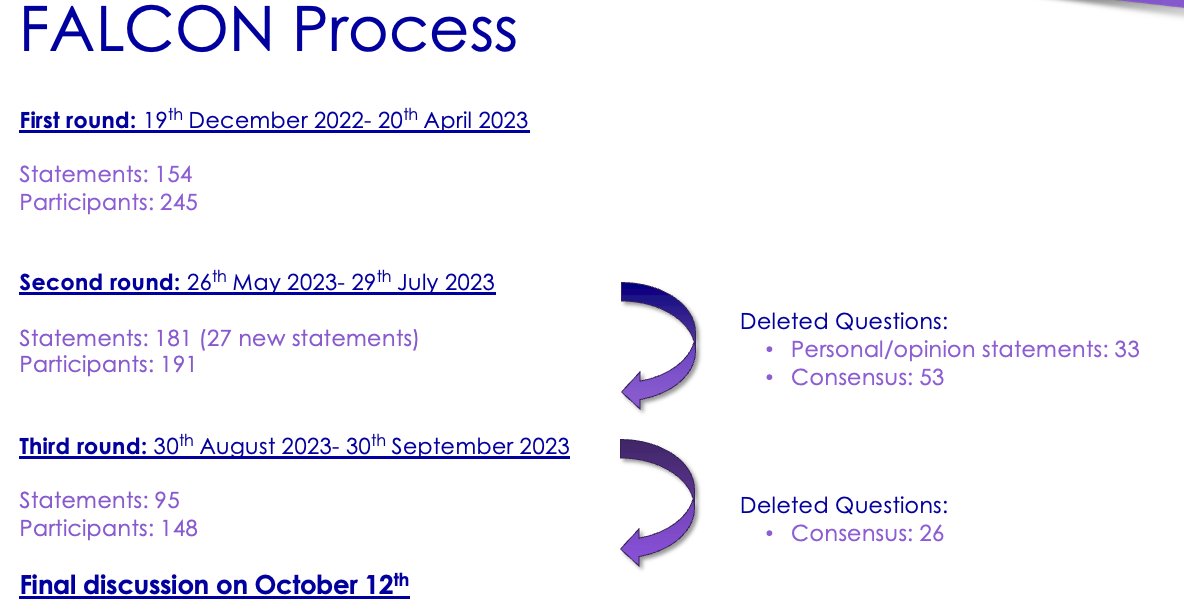
During the final discussion on October 12th, 2023, discussion of all the statements that reached consensus during the previous rounds resulted in subsequent minor changes. A 4th survey was completed by the attendees, with 69 statements assessed, of which 50 reached a consensus.
Subsequent additional discussion of the 19 remaining statements that did not reach a consensus after the short survey, led to an additional 7/19 reaching a consensus. As a result, 12 statements did not reach consensus.
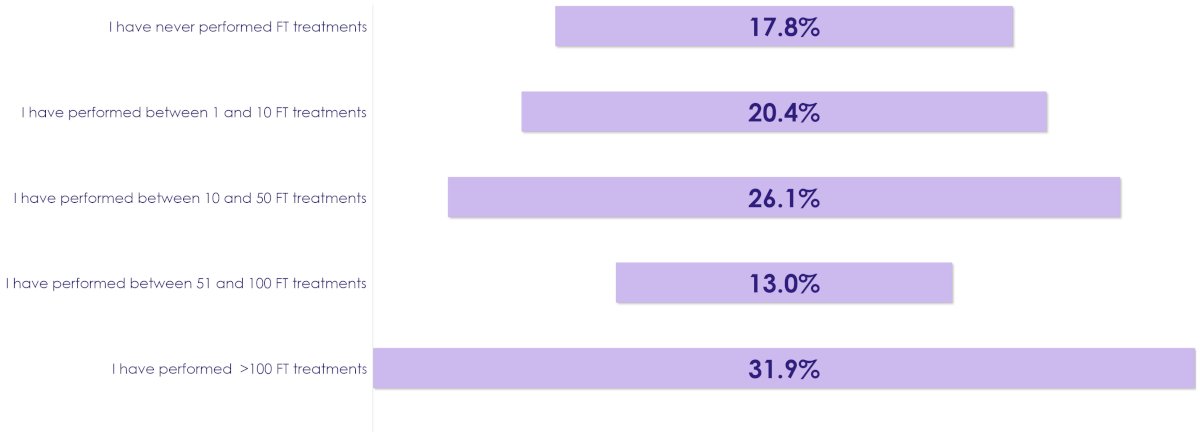
With regards to the respondents’ characteristics, their experience with performing focal therapy varied considerably:
With regards to patient selection criteria, the following consensus statements were reached:
- Life expectancy
- Life expectancy should be a determinant of focal therapy
- Age should not be a determinant
- Voiding symptoms
- Voiding symptoms do not contraindicated focal therapy
- Genetics
- Genomic tests results from biopsy might influence the decision to offer focal therapy
- Patients with BRCA gene mutation should not be offered focal therapy
- Tissue genomic tests should not be offered to all patients prior to focal therapy
- PSA
- PSA should be considered as an inclusion or exclusion criterion for focal therapy
- Histopathology
- Focal therapy should not be offered to patients with localized International Society of Urological Pathology (ISUP) 1 prostate cancer if they agree with active surveillance
- Focal therapy should be offered to patients with localized ISUP 2 (percentage of pattern 4 <10%) prostate cancer even if they agree with active surveillance
- If cribriform pattern is present, focal therapy should be considered over active surveillance
- Focal therapy should be offered to patients with localized ISUP 2 (percentage of pattern 4 >10%) prostate cancer
- Focal therapy should be offered to patients with localized ISUP 3 prostate cancers
- During the final discussion, there was an 89% agreement that focal therapy should be offered to these patients with localized ISUP 3 disease
- Focal therapy should not be offered to patients with localized > ISUP 3 prostate cancer
- Lesions
- All lesions can be treated with focal therapy with favorable oncological and functional outcomes regardless of their location if the lesion can be reached safely by the chosen energy
- Prostate volume does not matter If the lesion can be reached
- MRI and biopsy
- Local clinical stage should be based on MRI
- Focal therapy should not be offered in cases of extracapsular extension on MRI if highly likely
- ≥ 3 – 4 targeted + ≥ 10 – 12 systematic biopsies should be performed
- MRI in-bore or MRI/ultrasound fusion biopsies or cognitive fusion biopsies are permissible
- Focal therapy should not be offered in case of negative MRI and positive biopsies
- Focal therapy should not be offered if MRI is not available or if the quality is low
- PSMA-PET/CT is not considered a suitable replacement for MRI in patient selection for focal therapy
- The presence of positive biopsies outside the lesion detected on MRI does not contraindicate focal therapy
- Focal therapy may be offered to patients with multifocal MRI lesions
- If positive biopsies are found in one of multiple MRI-detected lesions, focal therapy should treat the confirmed lesion
With regards to treatment approach, the following consensus statements were reached:
- Treatment extension
- The minimal margin when treating the lesion is 5 mm
- A minimum safety margin of 10 mm would be unnecessary
- Hemiablation should not be considered the minimal extent of a focal treatment
- Energy selection
- No energy can be recommended over others in terms of effectiveness and safety
- Energy selection should be mainly based on the location of the tumor and operator's experience
- Margin
- Focal therapy may be performed if the lesion is <5 mm from the rectum
- A minimum safety margin of 10 mm from the rectum would be unnecessary
- Focal therapy should not be performed if the lesion is <5 mm from the sphincter
- A minimum safety margin of 10 mm from the sphincter would be unnecessary
With regards to follow-up, the following consensus statements were reached:
- Follow-up
- Patients should be followed up to 10 years by the urologist
- Patients should be offered more than one salvage focal therapy after the failure of the initial focal therapy
- Functional outcomes
- Functional outcomes must be assessed every 3 months for 1 year, then yearly until stability
- Functional outcomes should be assessed exclusively by validated questionnaires (such as EPIC, IPSS, and IIEF)
- Oncological outcomes
- PSA should be done 3-monthly for the first year, then 6-monthly
- There is no consensus on PSA failure definition after focal therapy
- MRI should be performed every 6 – 12 months initially, and subsequently on an annual basis
- ≥ 10 - 12 systematic plus ≥ 3 - 4 target biopsies should be done within 12 months post-treatment.
No consensus was reached for the following statements:
- Transperineal versus transrectal biopsies prior to focal therapy
- Substituting MRI with PSMA when MRI is neither possible nor available
- Possibility of treating non-visible lesions on MRI
- PSA threshold and the value of PSA density in selecting patients for focal therapy
- Focal therapy for bilateral lesions (cT2c)
- Acceptance of extracapsular extension on MRI for patients treated with focal therapy.
- Only if highly unlikely?
- The implications of the cribriform pattern in patient selection for focal therapy
- Minimum treatment extension: Beyond the margins, should a quadrant ablation be the minimum treatment extension?
- Definition of PSA failure after focal therapy
- The possibility of follow-up with MRI and PSA without control biopsies in centers with extensive experience in focal therapy
- The role of PSMA in follow-up after focal therapy
- Is PSMA superior to MRI?
Dr. Rodríguez Sánchez concluded by noting that the Falcon project serves as a comprehensive guide for focal therapy, from patient selection to follow-up. Furthermore, it has helped identify deficiencies in our knowledge that will guide future research in focal therapy.
Presented by: Lara Rodríguez Sánchez, MD, PhD, Urologic Surgeon Associate Assistant, Institut Mutualiste Montsouris, Ville de Paris, France
Written by: Rashid K. Sayyid, MD, MSc – Society of Urologic Oncology (SUO) Clinical Fellow at The University of Toronto, @rksayyid on Twitter during the 2023 Society of Urologic Oncology (SUO) Annual Meeting, Washington, D.C., Tues, Nov 28 – Fri, Dec 1, 2023.


