(UroToday.com) In a plenary session at the Society of Urologic Oncology Annual Meeting focused on early prostate cancer diagnosis and treatment, Dr. Caroline Moore and Dr. Daniel Spratt provided a point/counterpoint debate on the role of focal therapy for localized prostate cancer. Following Dr. Moore’s presentation, Dr. Spratt argued against focal therapy.
He began his talk by highlighting what he would NOT cover in further detail, namely the lack of quality data, the multi-focal biology of prostate cancer, and higher rates of recurrence reported following focal therapy. Notably, he emphasized that both guidelines and payers have stated, in the United States at least, that focal therapy is investigational.
He then argued that focal therapy as monotherapy would not exist if we were to be entirely patient focussed. This is because the goal of treatment, for any patient, is to improve the way a patient experiences life, considering both the quality and quantity of life. In this context, he highlighted data from the ProtecT trial demonstrating remarkably low prostate cancer-specific mortality, even with active monitoring. Thus, it is nearly impossible to consider that focal therapy could improve the quantity of life for a patient with localized prostate cancer.
Then, in the absence of an improvement in quantity of life, we must consider the potential for focal therapy to improve quality of life. This centers on patient-reported outcomes. Dr. Spratt then considered the quality of life outcomes of focal therapy compared to conventionally accepted treatment options including active surveillance, radical prostatectomy, and radiotherapy.
The quality of life burden associated with active surveillance, Dr. Spratt pointed out, rests in the surveillance burden. In consensus recommendations, he highlighted that the surveillance regime for a patient undergoing focal therapy is in fact more intensive than active surveillance.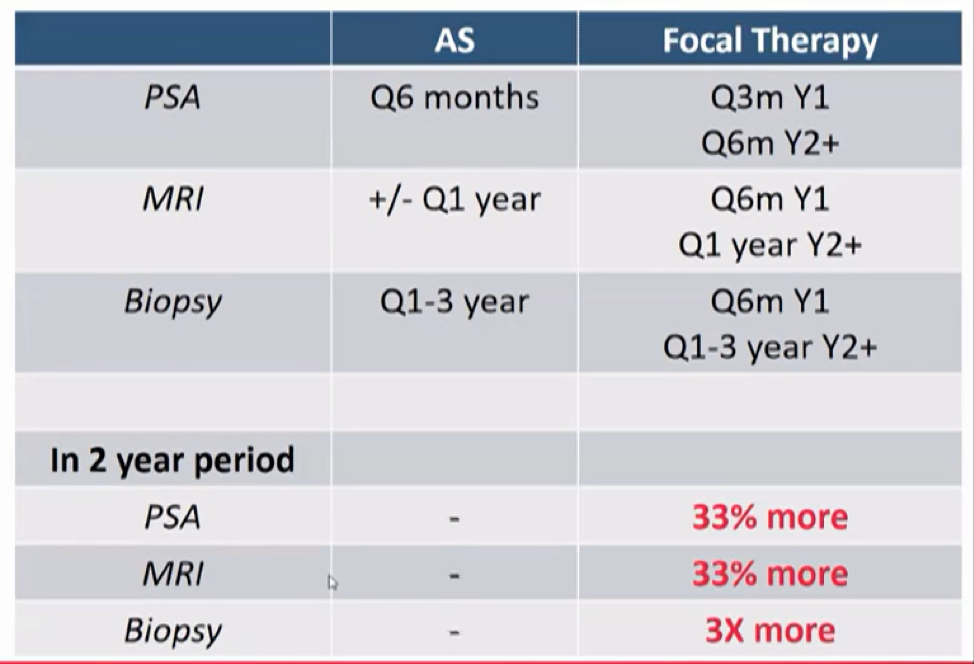
Thus, it is unlikely that focal therapy could have a higher quality of life compared to an active surveillance regime.
Dr. Spratt then highlighted a recent systematic review published in European Urology examining changes in focal therapy for prostate cancer over the past five years. Citing these data, he compared quality of life outcomes between radical prostatectomy and focal therapy. While focal therapy is associated with lower rates of urinary incontinence and erectile dysfunction, he emphasized that there is an increased burden of monitoring, higher rates of recurrence, and increased salvage therapy toxicity for patients who opt for focal therapy.
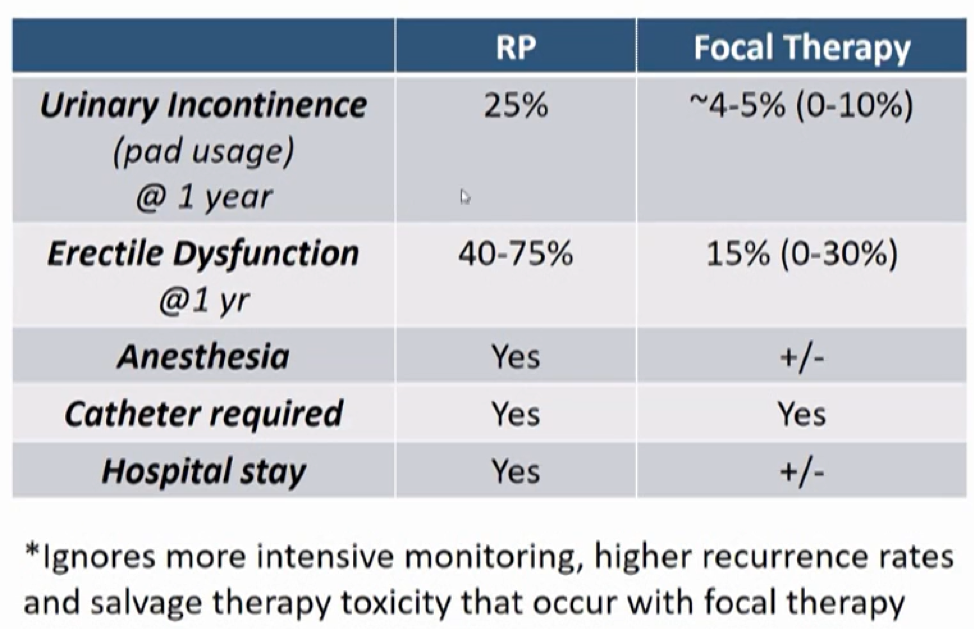
Finally, he compared quality of life for patients treated with focal therapy to radiotherapy. In this regard, he highlighted low rates of urinary incontinence and erectile dysfunction at 1 year for patients treated with external beam radiotherapy.
Thus, he postulated that focal therapy exists as a mechanism for urologists and radiologists who want to reduce the side effect profile compared to surgery. Instead, he suggested radiotherapy as an alternative approach. Potentially more cynically, he suggested that there may be a financial competitive advantage to offer these treatment approaches. To address this, he suggested removing financial incentives, though this is potentially primarily an American-based issue and approach.
Presented by: Daniel Spratt, MD, Vincent Smith Professor and Chair of Radiation Oncology, Case Western University


