(UroToday.com) In a plenary session of the Society of Urologic Oncology Annual Meeting focused on transperineal prostate biopsy, Dr. Arvin George discussed approaches we may consider for improving the detection of clinically significant cancer. In particular, he emphasized that this considers how transperineal biopsy may improve the yield of biopsy, particularly at the apex and anteriorly.
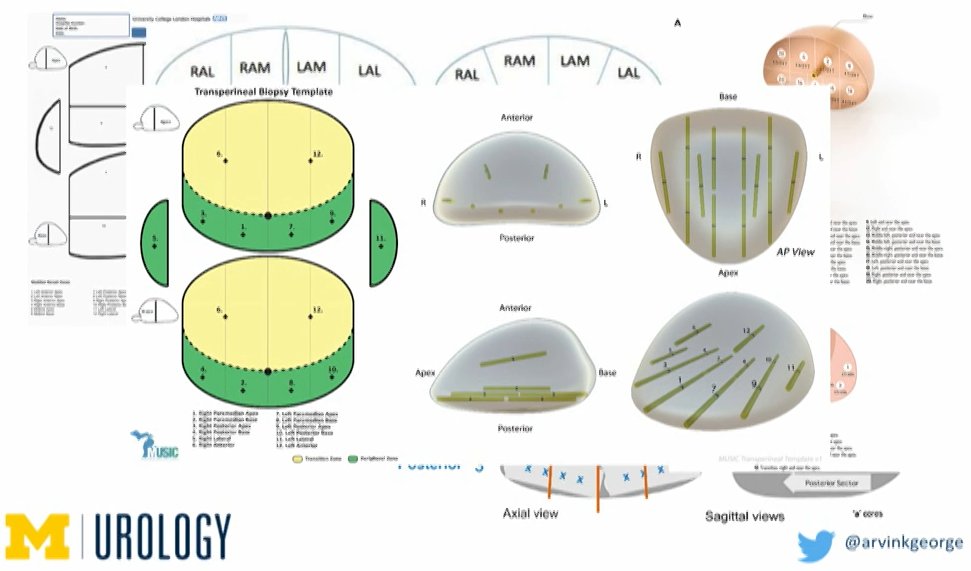
He first began by emphasizing the importance of transperineal templates, particularly as these differ from the approach used transrectally.
In the context of the Michigan Urological Surgical Improvement Collaborative (MUSIC), the overall cancer detection rate between transperineal (55.8%) and transrectal (54.6%) prostate biopsy is similar. When examining clinically significant prostate cancer (defined as grade group 2 or higher), rates were again not statistically different (34.5% vs 35.7%, p=0.5). He noted that, in this context, men with a negative multiparametric MRI were often undergoing transperineal biopsy whereas those with a positive MRI were undergoing a transrectal fusion biopsy.
Dr. George emphasized that, at least theoretically, transperineal biopsy should improve detection in the anterior prostate and minimize upgrading at the time of radical prostatectomy. He emphasized that, in the context of widespread utilization of mpMRI, the detection of disease in the anterior prostate based on transperineal biopsy may be a “moot point”. To this end, he emphasized that based on meta-analyses, the negative predictive value of MRI (defined as PI-RADS 1-2) is nearly 91% for excluding grade group 2 or greater and more than 97% for excluding grade group 3 or higher. If we operationalize a negative MRI as PI-RAD 1-3, these fall somewhat to 87% and 96%, respectively for excluding grade group 2 or greater and grade group 3 or greater. He emphasized that, at least in terms of anterior tumor detection, the use of upfront MRI mitigates the advantage of one biopsy technique over the other.
He then emphasized that, while fusion biopsy has traditionally been in the domain of transrectal biopsies, in the last two years there have been significant advances in terms of transperineal fusion biopsy.
Dr. George highlighted resources available through the MUSIC group which may allow physicians interested in transperineal biopsy to more easily initiate their program, including checklists, ordering information, templates, and technique videos. Additionally, there is a patient education video associated with transperineal prostate biopsy.
In summary, he emphasized that cancer detection rates for the two biopsy approaches are comparable. In particular, he highlighted that prostate MRI evens the playing field. Further, while we may reduce infectious complications from transrectal biopsy, transperineal biopsy is not going away.


