In this cohort study, patients who underwent bilateral inguinal lymph node dissection and had complete data were identified in a large multi-institutional international cohort from eight high volume referral centers in seven countries who were diagnosed with penile squamous cell carcinoma from 2000 to 2017. Recurrences were identified and stratified by site of recurrence, as well as timing of recurrence by site. Multivariable logistic regression analysis was used to determine associations with recurrence, and multivariable Cox regression analysis was used to determine associations with overall survival. Kaplan-Meier estimates and log-rank testing were used to compare survival functions by site of recurrence. A sub-group analysis of the distant recurrences analyzed timing of recurrence and OS by the specific site of distant recurrence.
There were 551 patients were included in the final study population, with a median age of 62 (IQR 52-70) years, who were most commonly pT2 (41%), with the most common primary procedure being partial penectomy (66%). Overall 176 (32%) patients recurred after inguinal lymph node dissection:
- Distant: 46%
- Local: 11%
- Inguinal: 25%)
- Pelvic: 18%
As follows is the Kaplan Meier estimate for RFS by site of recurrence among patients that recurred:
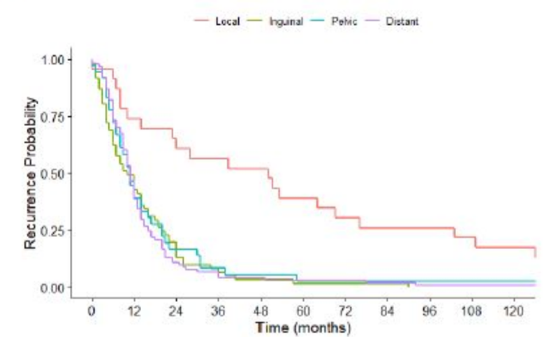
The median time to recurrence was 11 months for distant recurrences, 50 for local, 10 for inguinal, and 11 for pelvic. Greater than 95% of distant, inguinal, and pelvic recurrences occurred within 43 months of inguinal lymph node dissection, versus 152 months for local recurrences. Recurrence was associated with pT3/4 (OR 1.60, 95%CI 1.0-2.5), pN2 (OR 2.5, 95%CI 1.3-4.6), and pN3 (OR 6.4, 95%CI 3.9-11.0).
Patients who had a local recurrence had similar overall survival to patients with no recurrence (HR 0.97, 95%CI 0.4-2.4), and worse overall survival was identified in patients with inguinal (HR 4.39, 95%CI 3.0-6.4), pelvic (HR 3.03, 95%CI 1.8-5.0), or distant (HR 4.32, 95%CI 3.1-6.0) recurrences. Patients with distant lung recurrences had worse overall survival than other distant sites (HR 2.19, 95%CI 1.3-3.8).
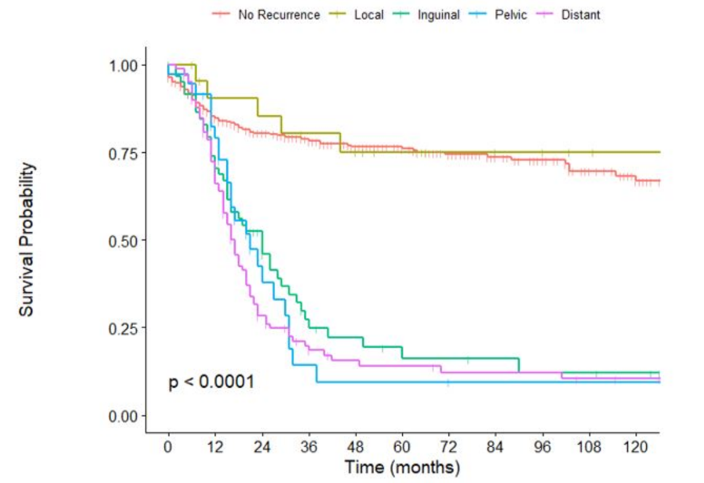
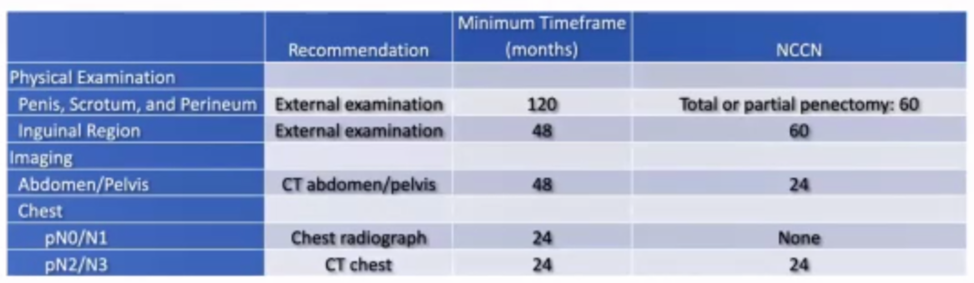
There were 32% of patients that had a post-inguinal lymph node dissection recurrence. Local recurrences occurred on a lengthy timeline, with 95% occurring within 152 months of inguinal lymph node dissection, stressing the necessity of very long-term follow up of the penis, perineum, and scrotum. Greater than 95% of distant, inguinal, and pelvic recurrences occurred within 43 months of inguinal lymph node dissection, suggesting that surveillance for these outcomes beyond this timeframe may be low yield. This data can be used to create evidence-based surveillance schedules:
In conclusion, inguinal, pelvic, and distant recurrences were confirmed to confer worse overall survival, and local recurrences had no effect on survival. Interestingly, patients with lung recurrences had significantly worse overall survival than those who recurred at other distant sites.
Presented by: Nicholas Chakiryan, MD, Moffitt Cancer Center, Tampa, FL
Co-Authors: Aaron Dahmen, Marco Bandini, Nick Watkin, Michael Ager, Maarten Albersen, Eduard Roussel, Yao Zhu, Ding-Wei Ye, Antonio A Ornellas, Oliver W Hakenberg, Axel Heidenreich, Friederike Haidl, Andrea Necchi, Philippe E. Spiess
Written by: Zachary Klaassen, MD, MSc – Assistant Professor of Urology, Georgia Cancer Center, Augusta University/Medical College of Georgia Twitter: @zklaassen_md at the 2020 Society of Urologic Oncology Annual Meeting – December 2-5, 2020 – Washington, DC


