Dr. Anne P. Cameron shows the audience that far too many antibiotics are being used in the clinic. Bacteria are ubiquitous and not all bacteria are not “bad”. She shows that bacteria are in fact essential to the ecosystem. She asks, “are antibiotics the new opioids”? We live in an era of informed consent and are we moving towards consenting patients before the use of antibiotics?
She shows the development of antibiotic resistance over time. The 1950s-1970s were a golden era of antibiotics however in recent time development has decreased. The overuse of antibiotics leads to resistance of bacteria globally. She gives two examples of antibiotic resistance. In 2009, there was a strain of Gonorrhea that was resistant to all antibiotics. A woman died of sepsis due to a strain of bacteria resistant to all antibiotics.
Even using low dose prophylaxis can lead to resistance over time. A recent publication by Stalenhoef shows that patients who have recurrent UTIs from multidrug-resistant bacteria benefit from gentamicin bladder irrigations and over time can even decrease resistance from 78% to 23%.
Asymptomatic bacteruria exists in 30%-90% of patients who catheterize. These patients should not necessarily undergo treatment. There are certain times when asymptomatic bacteruria should be treated, these are the pregnant patient and those who will be undergoing urinary tract manipulation (cystoscopy).
The AUA best practice statement recommends a fluoroquinolone antibiotic or trimethoprim-sulfamethoxazole in all patients undergoing cystourethroscopy and in patients with risk factors undergoing urodynamics. However, she showed several studies that with no antibiotic use there was no significant increased risk of UTI, in particular, the one by Clennon et al. 2019. She talks about the rates of UTI after bladder botulinum toxin injections. Mouttalib 2010 showed a 7.1% rate of UTI and Leitner 2016 showed 7% UTI rate in patients with bacteruria and 5% in sterile urine. She has also developed a protocol for use of antibiotics in selective UDS patients.
The population of patients with asymptomatic bacteruria has been studied with 2 randomized control trials and 2 prospective non-randomized trials showing antibiotic treatment significantly reduced symptomatic UTIs.
Dr. Kauffman emphasizes antibiotic stewardship vs antibiotic abstinence. These two terms are not synonymous. Stewardship should be practiced and coordinated for the appropriate patient.
She discusses when antibiotics are recommended in urodynamics procedures. The patient with abnormal genitourinary anatomy, neurogenic lower urinary tract dysfunction, elevated PVRs (50-100 cc), patients older than 70, asymptomatic bacteruria, immunosuppressed, catheterization (indwelling or CIC), total joint replacement. She does not recommend antibiotic use in the following patients.
She also shows the results of ROSETTA trial that patients undergoing bladder Botox injections had a 36% rate of symptomatic UTI with Cipro 500 mg post procedure and for 3 days arguing for the use of antibiotics.
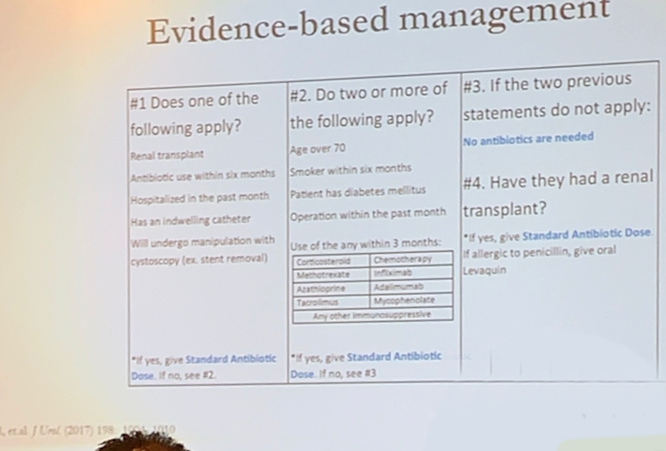
She concludes that using evidence-based management to practice antibiotic stewardship in the office decrease rates of symptomatic UTI.
Moderator: Michael J. Kennelly, MD, FACS, FPMRS, Urology, Urogynecology, Female Pelvic Medicine and Reconstructive Surgery, Spinal Cord Injury Medicine, Atrium Health
Written by: M Lira Chowdhury, DO, Fellow, Female Urology, Pelvic Reconstructive Surgery & Voiding Dysfunction, The University of California Irvine, Department of Urology, @lirachowdhury at the Society of Urodynamics, Female Pelvic Medicine & Urogenital Reconstruction Winter Meeting, SUFU 2019, February 26 - March 2, 2019, Miami, Florida


