Precision Point Specialty Analytics Portal, an electronic medical record database covering over 2.4 million community-based urology patients, was used to identify adult patients diagnosed and treated for non-neurogenic OAB between January 1, 2015, and December 31, 2019. Identification was through ICD-9, ICD-10, and procedure codes. Included in the analysis were patients with a minimum of two OAB clinic visits at least 30 days apart. A subset of eligible patients was randomly selected and stratified into navigation and non-navigation groups. Treatment continuation was defined as retreatment within 12-months.
This retrospective analysis yielded a total of 9,000 patients (navigated care [n=1,151] and non-navigated care [n=7,849]) randomly selected from the 170,000 patients who met all study inclusion criteria. Navigated-care and non-navigated care patients were most likely to be treated at a medium sized urology practice (34.9% and 35.8%, respectively). Mean age at diagnosis (index date) was 63.5 ± 16.9 years (64.0 navigated and 63.5 non-navigated) and 59.9% of patients were female (81.7% navigated vs. 56.7% non-navigated; p <0.001).
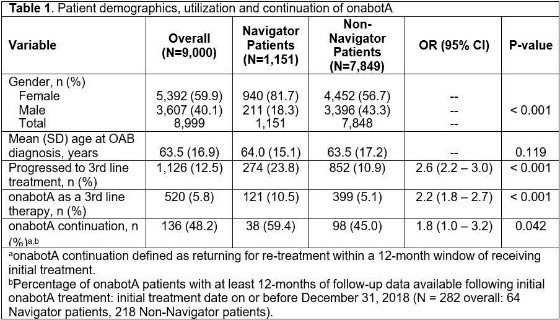
Navigated care was more likely to advance patients to a third line treatment or specifically to onabotA versus non-navigated care (both p <0.001; Table 1) and the proportion of patients continuing onabotA treatment significantly improved with navigated care versus non-navigated care (p=0.042; Table 1).
The authors concluded that navigated patient-centered care can significantly increase utilization of third line treatment options such as onabotA and improved treatment continuation.
Presented by: Raveen Syan, MD,1 Jennifer Miles-Thomas, MD,2 Diane K. Newman, DNP, FAAN, BCB-PMD,3 Nitya Abraham, MD,4 Keely Madaj, MPH,5 Krystal Anson Spenta, MPH,6 Amin Boroujerdi, PhD,6 Zhanying Bai, MS,7 Lei Luo, MPH,7 Ekene Enemchukwu, MD, MPH8
- University of Miami Miller School of Medicine, Miami
- Urology of Virginia, Virginia Beach
- University of Pennsylvania Perelman School of Medicine, Philadelphia
- Montefiore Medical Center, Bronx
- PPS Analytics, Independence
- AbbVie, Irvine, CA
- AbbVie, Madison, NJ
- Stanford University School of Medicine, Stanford
Written by: Diane K. Newman, DNP, ANP-BC, FAAN, Adjunct Professor of Urology in Surgery, Perelman School of Medicine, University of Pennsylvania and Co-Director of the Penn Center for Continence and Pelvic Health at the 2022 Society of Urodynamics, Female Pelvic Medicine & Urogenital Reconstruction (SUFU) Winter Meeting, February 22 - 26, 2022


