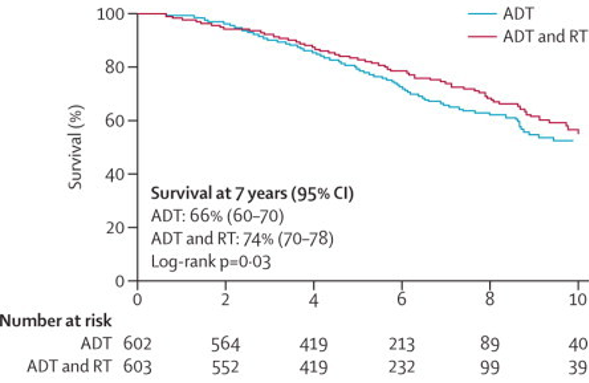
Dr. Clarke then discussed the PR07 Phase III clinical trial assessing combined androgen deprivation therapy (ADT) and radiation therapy for locally advanced prostate cancer.1 This trial had 1,057 men with T3 or T4 prostate cancer, or T2 disease with either a PSA more than 40 ng/mL (n=119) or PSA more than 20 ng/mL and a Gleason score of 8 or higher (n=25). Patients were randomly assigned to received lifelong ADT (n=602) and ADT plus radiation therapy (n=603). Over a median follow-up was 6.0 years (IQR 4.4-8.0), a total of 320 patients had died, 175 in the ADT only group and 145 in the ADT plus radiation therapy group. The addition of radiation therapy to ADT improved overall survival at 7 years (74%, 95% confidence interval [CI] 70-78 vs 66%, 60-70; hazard ratio [HR] 0.77, 95% CI 0.61-0.98, p=0.033)
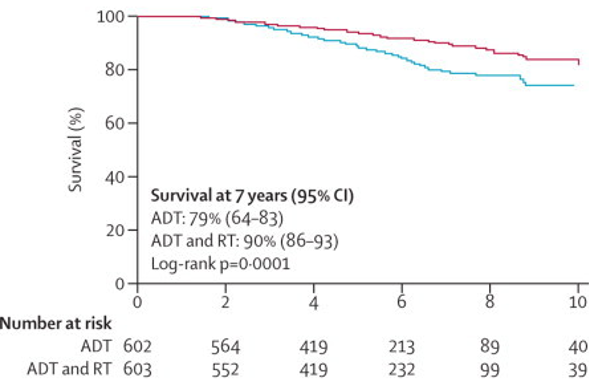
as well as improved prostate cancer specific survival at 7 years (90%, 95% CI 86-93 vs 79%, 95% CI 64-83; HR 0.54, 95% CI 0.27-0.78, p=0.0001):
Dr. Clarke notes that these results are both excellent – if we had used modern imaging in these patients, the classical staging would have looked much different. In the proPSMA trial, Dr. Clarke notes that the patients were very similar to those enrolled in PR07 with biopsy-proven prostate cancer and high-risk features.2 There were 302 men randomly assigned to conventional imaging (n=152) and PSMA PET-CT (n=150). PSMA PET-CT had a 27% (95% CI 23-31) greater accuracy than that of conventional imaging (92% [88-95] vs 65% [60-69]; p<0.0001). Additionally, this trial found a lower sensitivity (38% [24-52] vs 85% [74-96]) and specificity (91% [85-97] vs. 98% [95-100]) for conventional imaging compared with PSMA PET-CT.
So, should we redefine our clinical staging and treatment planning based on this data? Dr. Clarke notes that there are three rules of research: "Is it New?", "Is it True?", "Does it Matter?". Regarding whether it is new or true, Dr. Clarke highlights that in the surgical literature among patients with high PSAs (>20) and high Gleason grade (>80%), the lymph node metastasis rate is likely greater than 80%. So, the findings in proPSMA are true, but they don’t really tell us anything new, according to Dr. Clarke, given that lymph node positivity is a common event in high-risk radical prostatectomies. Regarding the third question, does it matter, Dr. Clarke notes that in the proPSMA study, conventional imaging conferred management change with a high or medium effect in 23 men (15%; 95% CI 10–22), compared with 41 men (28%; 21–36) who underwent first-line PSMA PET-CT (p=0·008). Following first-line PSMA PET-CT, 20 (14%) of 148 patients were directed from curative to palliative-intent treatment, 11 (7%) had a change in radiotherapy technique, and 11 (7%) in surgical technique. Thus, there is a Will Rogers effect on stage and treatment migration, which will change the way we view these patients and how we treat them.
Dr. Clarke highlights that this matters by discussing data from the STAMPEDE trial and the impact of radical radiotherapy. Time to failure-free survival was worse in patients with N+ disease (HR 2.02, 95% CI 1.46-2.81) than in those with N0 disease. Failure-free survival outcomes favored planned use of radiotherapy for patients with both N0M0 (HR 0.33, 95% CI 0.18-0.61) and N+M0 disease (HR 0.48, 95% CI 0.29-0.79).3 Thus, if these patients had been upstaged to N+ disease with PSMA PET-CT, Dr. Clarke suggests they may have been treated quite differently. Similarly, in the STAMPEDE analysis of radiotherapy to the primary tumor for newly diagnosed metastatic prostate, radiotherapy improved failure-free survival (HR 0.76, 95% CI 0.68-0.84; p<0.0001) but not overall survival (HR 0.92, 95% CI 0.80-1.06; p=0.266).4
Should we shift to novel imaging? Dr. Clarke quoted Buxton's Law and the Medical Tipping Point to note that “it is always too early (for rigorous evaluation) until, unfortunately, it is suddenly too late”:
Dr. Clarke summarized by highlighting that oligometastatic disease should be defined based on standard imaging modalities and that new imaging modalities need to be further assessed in clinical trials to establish exactly what their utility is on treatment and patient outcomes.
Presented by: Noel William Clarke, MD, Consultant Urologist, Salford Royal Hospital and The Christie Hospital, Manchester, United Kingdom
Written by: Zachary Klaassen, MD, MSc, Assistant Professor of Urology, Georgia Cancer Center, Augusta University/Medical College of Georgia, Augusta, Georgia, Twitter: @zklaassen_md at the 2020 Société Internationale d'Urologie Virtual Congress (#SIU2020), October 10th - October 11th, 2020
References:
1. Warde, Padraig, Malcolm Mason, Keyue Ding, Peter Kirkbride, Michael Brundage, Richard Cowan, Mary Gospodarowicz et al. "Combined androgen deprivation therapy and radiation therapy for locally advanced prostate cancer: a randomised, phase 3 trial." The Lancet 378, no. 9809 (2011): 2104-2111.
2. Hofman, Michael S., Nathan Lawrentschuk, Roslyn J. Francis, Colin Tang, Ian Vela, Paul Thomas, Natalie Rutherford et al. "Prostate-specific membrane antigen PET-CT in patients with high-risk prostate cancer before curative-intent surgery or radiotherapy (proPSMA): a prospective, randomised, multi-centre study." The Lancet (2020).
3. James, Nicholas D., Melissa R. Spears, Noel W. Clarke, David P. Dearnaley, Malcolm D. Mason, Christopher C. Parker, Alastair WS Ritchie et al. "Failure-free survival and radiotherapy in patients with newly diagnosed nonmetastatic prostate cancer: data from patients in the control arm of the STAMPEDE trial." JAMA oncology 2, no. 3 (2016): 348-357.
4. Parker, Christopher C., Nicholas D. James, Christopher D. Brawley, Noel W. Clarke, Alex P. Hoyle, Adnan Ali, Alastair WS Ritchie et al. "Radiotherapy to the primary tumour for newly diagnosed, metastatic prostate cancer (STAMPEDE): a randomised controlled phase 3 trial." The Lancet 392, no. 10162 (2018): 2353-2366.
Related Content:
Read the Opposing Debate: SIU Virtual Congress 2020: Debate: Imaging in the Definition of Oligometastatic Prostate Cancer - Oligometastatic Disease Should be Defined Based on Novel Imaging Modalities
Watch:PSMA PET/CT Imaging for Staging High-risk Prostate Cancer Prior to Curative-intent Surgery or Radiotherapy (proPSMA) - Michael Hofman and Declan Murphy
Read:EAU 2020: ProPSMA Study: A Prospective Randomised Multi-Centre Study of PSMA-PET/CT Imaging for Staging High Risk Prostate Cancer Prior to Curative-Intent Surgery or Radiotherapy


