Dr. Pettaway notes that it is clear that the presence and extent of inguinal lymph node metastasis dictates survival for patients with penile cancer. For example, those undergoing surgery with limited unilateral inguinal metastases (one to two unilateral nodes) have a 5-year disease-free survival of >70%. However, for patients with ≥3 unilateral or bilateral metastases, 5-year disease-free survival decreases to 12-60%. Furthermore, those patients with extranodal cancer extension (5-6% 5-year disease-free survival) or pelvic lymph node metastasis (10% 5-year survival) are rarely cured with surgery alone. Thus, it is indicated to perform an inguinal lymph node dissection for patients with palpable inguinal adenopathy and recommended for patients with no palpable adenopathy if they have ≥T1G2 (European Association of Urology [EAU]) or ≥T1b (National Comprehensive Cancer Network [NCCN]) penile tumors.
According to the TNM 8th edition for penile cancer, the following stages have corresponding pN+ risk:
- T1a: pN+ 10-18%
- T1b: pN+ 33-50%
- T2: pN+ 33-35%
- T3-T4: pN+ 49-53%
Dr. Pettaway highlighted that when lymph nodes are detected early and they are appropriately treated surgically, there is curative potential. The boundaries of the inguinal region are the sartorius muscle laterally, adductor longus muscle medially, the apex of the femoral triangle inferiorly, and 2 cm above the inguinal ligament superiorly. Several strategies have been developed to minimize the morbidity of penile cancer staging, including dynamic sentinel node biopsy, superficial/fascial sparing dissections, as well as laparoscopic/robotic approaches.
Dynamic sentinel node staging includes injecting technetium labeled sulfur colloid dye into the dermal lymphatics of the penis, which then spreads bilaterally to the inguinal lymph nodes. Intraoperatively, using the gamma probe, one is able to identify the sentinel lymph node, which is made easier to visualize during dissection if a blue dye is used (blue-stained node). After removing the node, a final scan of the area with the gamma probe is performed to ensure there is no additional activity. Dr. Pettaway notes that since you are only taking out several nodes when performing dynamic sentinel node biopsy, the complication rates are low, at ~10% in the majority of series. At high-volume centers, the sensitivity for detecting lymph node metastases is >90%: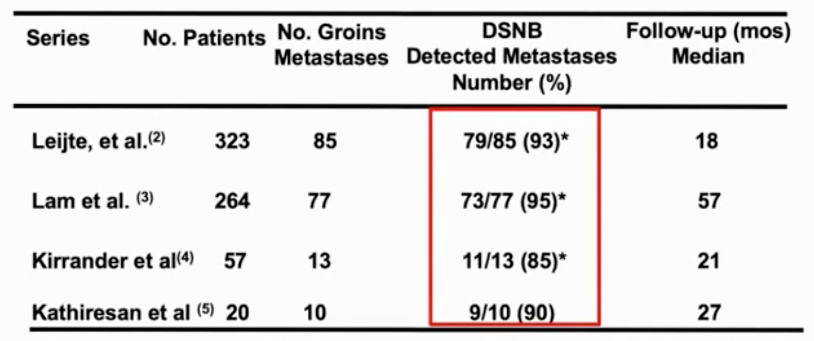
Dr. Pettaway prefers to do a superficial inguinal lymph node dissection, which involves removing the nodal tissue above fascia lata (midpoint of the sartorius and adductor longus muscles), and 2-3 cm above the inguinal ligament and apex of the femoral triangle, which identifies all “first echelon” lymph nodes. The benefit of this approach is that the saphenous vein and fascia lata are spared. It is important in this setting to perform frozen sections because if a superficial node is positive, one has to then perform a deep dissection. This is a very effective approach as Dr. Pettaway nodes that in patients with pN0 superficial nodes, he has never had an in-field recurrence.
Another effective approach is a fascial sparing complete inguinal lymph node dissection. This includes a superficial dissection but also includes nodes in the fossa ovalis (deep), which also spares the saphenous vein. Since you are getting those additional deeper nodes, there is no need to do frozen sections. In a series from China, Yao et al.1 performed 201 inguinal dissections with preservation of the fascia lata in 104 patients with clinical disease staged at ≤N2. A mean number of 12.5 nodes were removed per groin. One patient (1%) had a recurrence outside the borders of the fascia lata after seven months of follow-up, and the 3-year disease-free survival rate was 92.1% (100% for pN0, 91.3% for pN1, 80% for pN2, and 33.3% for pN3 disease).
With regards to complications of inguinal lymphadenectomy, superficial dissection has a complication rate of 50% per patient and 23% per groin, whereas, for the fascia sparing dissection, the total complication rate per patient is 57% and 29% per groin. For both techniques, the majority of these complications were minor.
Dr. Pettway states that laparoscopic and robotic inguinal lymphadenectomies are becoming more popular. The early goals of these techniques were to establish feasibility and adequacy of node removal, whereas more current goals are to assess complication rates and disease control rates. The following table summarizes the laparoscopic versus open inguinal lymphadenectomy series: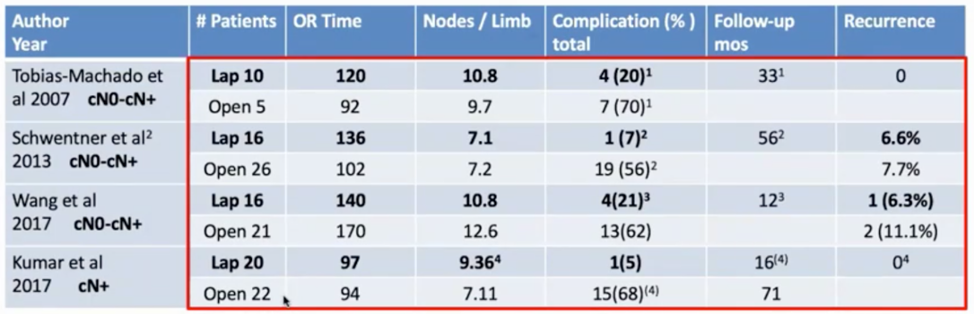
Similarly, there are two studies that have reported a comparison of outcomes among patients undergoing robotic versus open inguinal lymphadenectomy: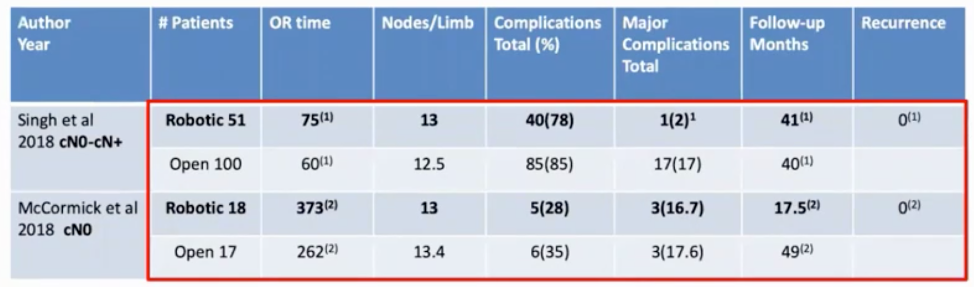
Early data for both laparoscopic and robotic approaches shows encouraging outcomes compared to the traditional open approach.
For patients with clinically palpable lymph nodes, Dr. Pettaway states that these are the patients that have the potential to die of their disease. In a study from Dr. Pettway’s group, 182 men underwent lymph node dissection for squamous cell carcinoma, with a median follow-up of 4.2 years.2 After lymph node dissection 34 men had a regional recurrence, of which 24 developed isolated regional recurrences without distant metastasis. The median recurrence-free survival (RFS) was 5.7 months, and the 3-year RFS rate was 70%. The 3-year RFS for patients with cN0, cN1, cN2, and cN3 disease was 91.7%, 64.5%, 54.7%, and 38.3%, respectively. Additionally, for men with ≥3 involved nodes, the 3-year RFS was 17% vs 82.4% in men with <3 involved nodes.
As such, for patients with cN+ nodes, adjuvant therapy is recommended. The EAU guidelines recommend upfront surgery for patients with cN1/cN2 disease followed by adjuvant chemotherapy (not adjuvant radiation). The NCCN guidelines take a slightly different approach, recommending upfront surgery for those with unilateral <4 cm nodes, followed by adjuvant chemotherapy, radiotherapy, or chemoradiotherapy. With regards to neoadjuvant therapy for cN+ patients, the EAU guidelines recommend neoadjuvant chemotherapy for men with fixed or pelvic lymph nodes, followed by inguinal lymphadenectomy for those patients that are responders. The NCCN guidelines take a broader approach, recommending neoadjuvant chemotherapy for those with ≥4 cm lymph nodes or bilateral disease.
Given this lack of level 1 data, the International Penile Advanced Cancer Trial (InPACT) may provide stronger evidence for how we should integrate therapy for these patients. The trial schema for the InPACT trial is as follows: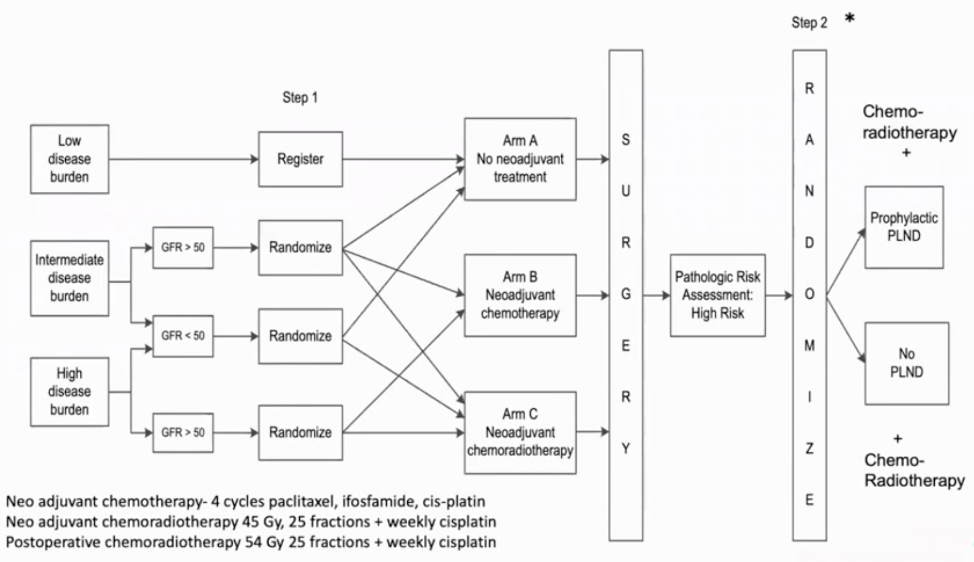
Discussing pelvic lymph node metastases, Dr. Pettaway notes that the risk of pelvic lymph node metastases is directly related to the status of the inguinal lymph nodes. As such, predictors of pelvic lymph node metastases are ≥2 positive inguinal nodes, as well as those with positive nodal extracapsular extension. If these predictors are positive, Dr. Pettaway advocates for a prophylactic pelvic lymph node dissection, which can be done in a minimally invasive fashion.
Dr. Pettaway concluded his presentation with the following take-home messages:
- Micro-metastatic penile cancer is curable with surgery
- Strategies to decrease morbidity including dynamic sentinel node biopsy, superficial, and fascia sparing dissections, as well as laparoscopic/robotic approaches
- Clinically palpable metastases are lethal
- The InPACT trial is a priority for assessing the efficacy of neoadjuvant therapy and the role of prophylactic pelvic lymphadenectomy
Presented by: Curtis A. Pettaway, MD, Professor, Department of Urology, Division of Surgery, The University of Texas MD Anderson Cancer Center, Houston, Texas
Written by: Zachary Klaassen, MD, MSc, Assistant Professor of Urology, Georgia Cancer Center, Augusta University/Medical College of Georgia, Augusta, Georgia, Twitter: @zklaassen_md at the 2020 Société Internationale d'Urologie Virtual Congress (#SIU2020), October 10th - October 11th, 2020
References:
1. Yao, Kai, Zi-jun Zou, Zai-shang Li, Fang-Jian Zhou, Zi-Ke Qin, Zhuo-Wei Liu, Yong-Hong Li, and Hui Han. "Fascia lata preservation during inguinal lymphadenectomy for penile cancer: rationale and outcome." Urology 82, no. 3 (2013): 642-647.
2. Reddy, Jay P., Curtis A. Pettaway, Lawrence B. Levy, Lance C. Pagliaro, Pheroze Tamboli, Priya Rao, Isuru Jayaratna, and Karen E. Hoffman. "Factors associated with regional recurrence after lymph node dissection for penile squamous cell carcinoma." Bju international 119, no. 4 (2017): 591-597.


