Athens, Greece (Urotoday.com) Dr. Alessandro Volpe gave an overview of the current role of cytoreductive nephrectomy in renal cell carcinoma (RCC).
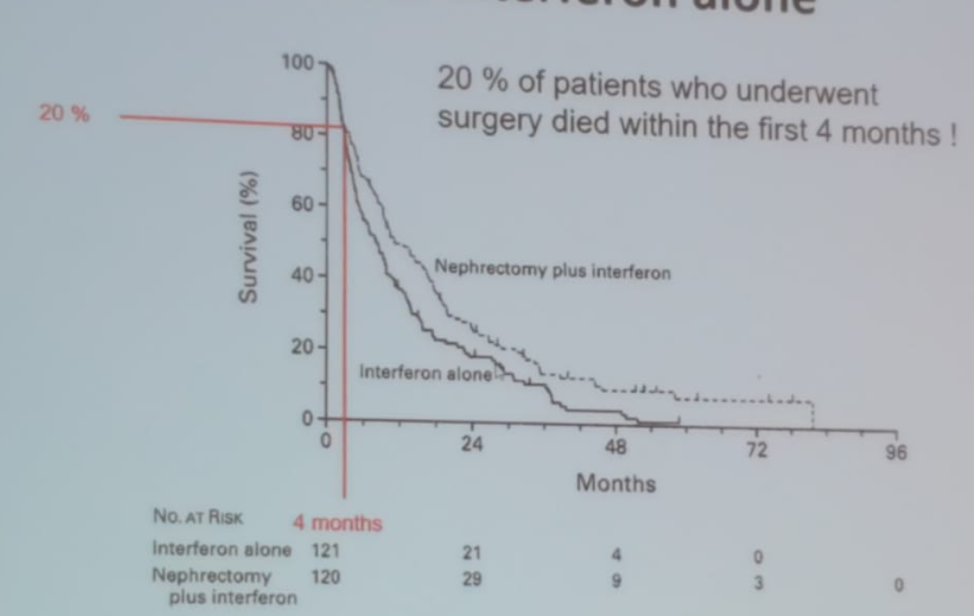
Up to one third of patients with RCC will present with metastatic disease. The concept of cytoreductive nephrectomy for metastatic RCC patients received significant recognition with the publication by Dr. Robert Flanigan’s paper in 2001 in the New England Journal of Medicine1. In this study, metastatic RCC patients who were treated with interferon-alpha and nephrectomy did better than those who were treated with only interferon alpha1. However, 20% of patients who underwent cytoreductive nephrectomy for metastatic RCC still died within the first 4 months (Figure 1).
Figure 1 – Actuarial survival among all patients in the Flanigan trial comparing interferon-alpha + nephrectomy to interferon-alpha alone:
In the current era, data from the United Kingdom show that cytoreductive nephrectomies consist of 4.6% of all nephrectomies performed and retrospective data have shown a clear advantage in patients undergoing cytoreductive nephrectomy compared to those who did not. However, these are retrospective data with its inherent limitations, including a clear selection bias, where the favorable patients are referred for cytoreductive nephrectomy compared to those with the more aggressive disease.
The problem with metastatic RCC is that it is a heterogeneous disease with varying degrees of feasibility regarding the ability to resect the primary tumor, feasibility of metastatic resection, burden of metastatic disease, histologic subtype, performance status, prognostic risk category, and symptoms. Patient selection for cytoreductive nephrectomy is key for success. That is why various criteria have been formulated to calculate and ascertain which patients will be better candidates for cytoreductive nephrectomy.
One of those risk criteria is the Heng criteria, conferring worse results and showing a clear overall survival difference between patients with favorable, intermediate and poor-risk (Figure 2). The Heng criteria include:
- Kranofsky performance status <80%
- Anemia
- Thrombocytopenia
- Neutropenia
- Hypercalcemia
- Time from diagnosis to treatment< 1 year
Figure 2 – Overall survival difference between favorable, intermediate, and poor-risk Heng criteria:
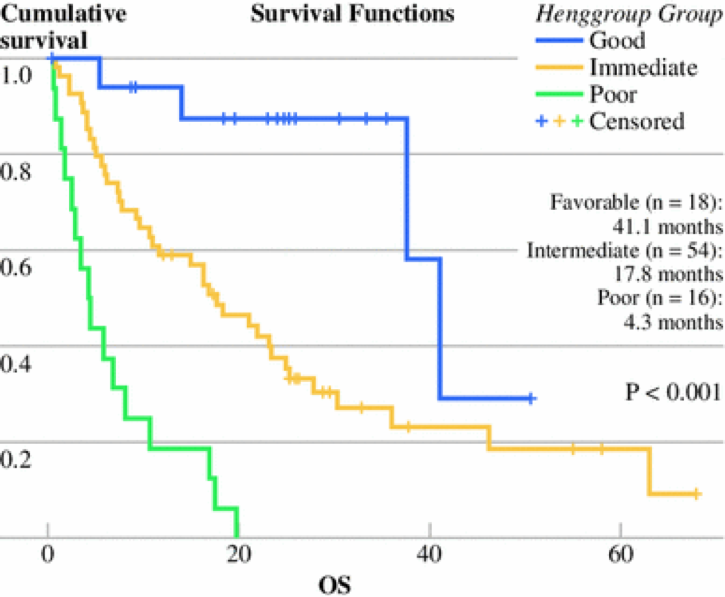
It is clear, using any type of criteria, that patients with poor-risk have no survival benefit when they undergo cytoreductive nephrectomy. Therefore, the 2018 EAU guidelines recommended offering cytoreductive nephrectomy only to favorable and intermediate-risk patients with metastatic RCC, as opposed to poor-risk patients.
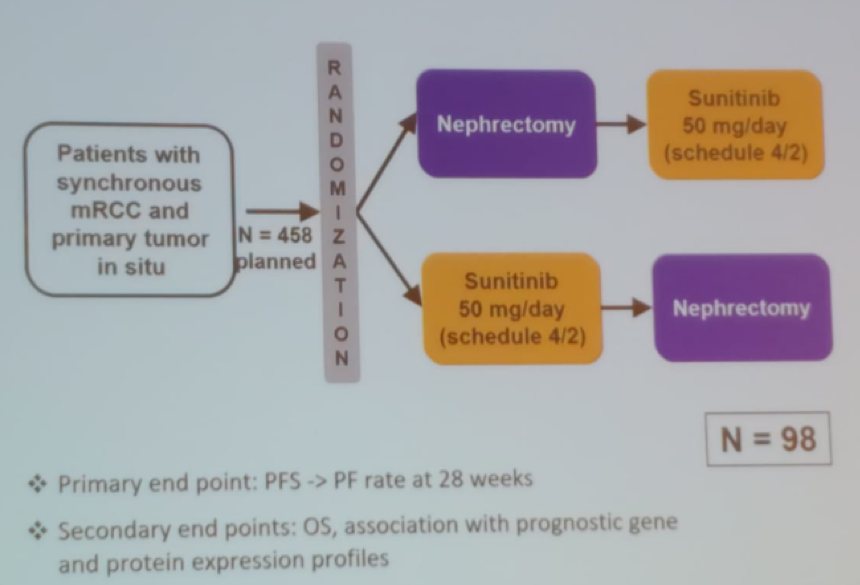
The SURTIME study, was a phase 3 study investigating the sequence of nephrectomy and sunitinib in metastatic RCC patients (Figure 3). Unfortunately, the trial accrued poorly and therefore the results were mainly exploratory. The results demonstrated that the sequence of cytoreductive nephrectomy and sunitinib did not affect the progression-free survival (PFS) at 28 weeks. The deferred cytoreductive nephrectomy approach used in the trial appeared to select outpatients with inherent resistance to systemic therapy. Furthermore, surgery appeared to be safe after treatment with sunitinib.
Figure 3 – SURTIME study design:
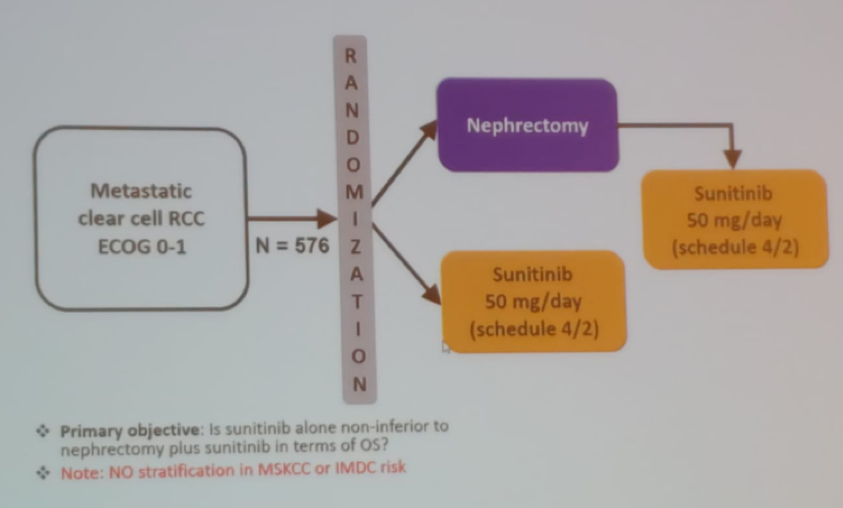
The most recent landmark trial, the CARMENA trial (Figure 4) was a phase 3 study of sunitinib only vs. nephrectomy followed by sunitinib2. The main limitations of this study included:
- 450 patients vs. 576 patients randomized (8 years vs. 4 years)
- 326 patients vs. 456 events (deaths)
- 7/patients recruited/center/year – a significantly low number of patients
- There was relevant crossover between the two arms
- There was a high proportion of poor-risk patients (44% vs. 41%).
Figure 4 – CARMENA study design:
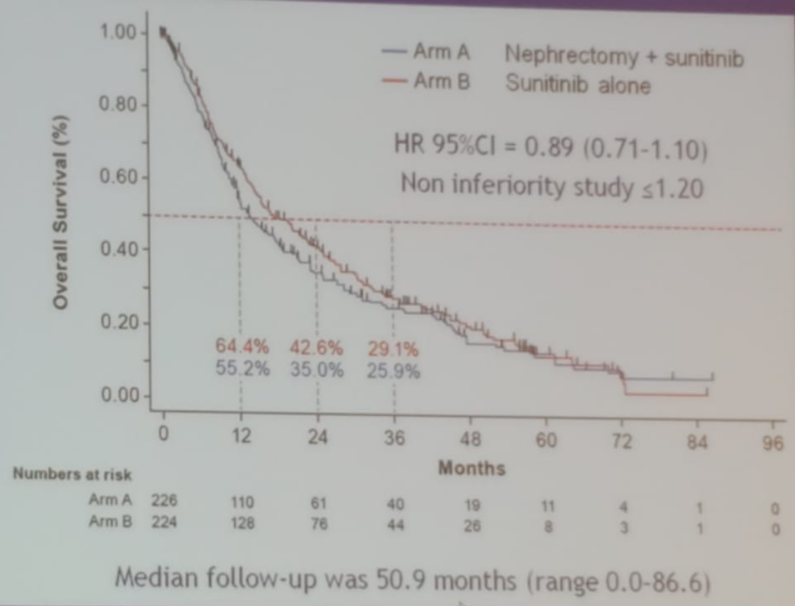
This trial showed no overall survival difference between the two arms after a median follow-up time of 50.9 months (figure 5)
Figure 5 – Overall survival in the CARMENA trial:
Due to the results of the CARMENA trial, the updated EAU guidelines on the treatment of metastatic RCC patients3 continue to recommend to not perform cytoreductive nephrectomy for poor-risk patients. Furthermore, for intermediate-risk patients who are asymptomatic and require systemic therapy, there is also a clear recommendation not to perform cytoreductive nephrectomy. Delayed cytoreductive nephrectomy is indicated in patients under VEGFR-TKI therapy who derive long-term sustained benefit and / or minimal residual metastatic burden. Immediate cytoreductive nephrectomy is recommended in patients with good performance status who do not require systemic therapy.
An updated treatment algorithm, courtesy of Dr. Axel Bex, is shown in Figure 6, including recommendations when to perform cytoreductive nephrectomy after immunotherapy in Table 1.
Figure 6 – Treatment algorithm for metastatic RCC patients:
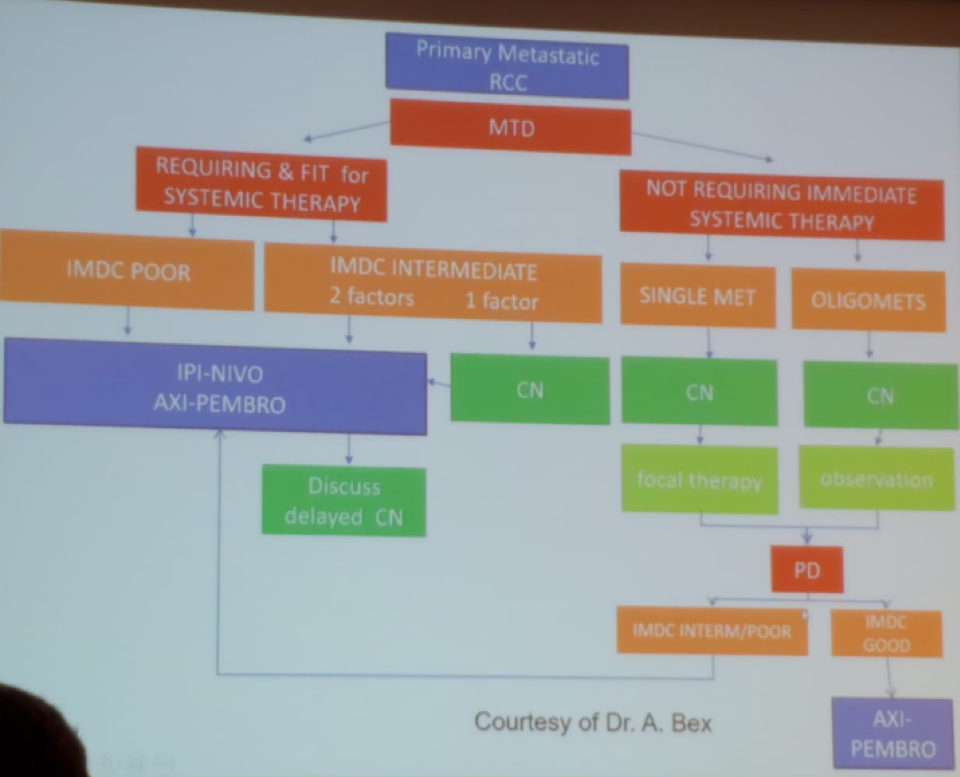
Table 1 – When to perform cytoreductive nephrectomy after immunotherapy:
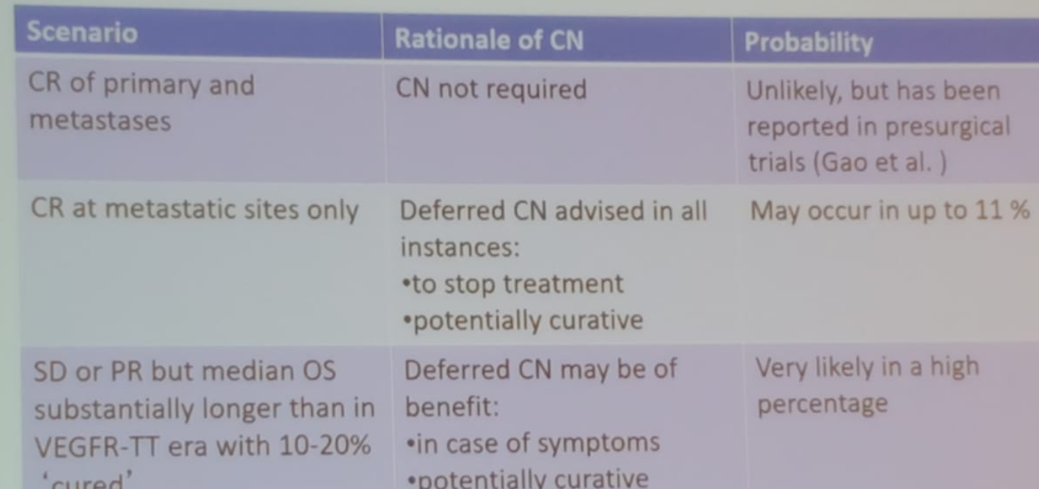
In conclusion, primary metastatic RCC is a heterogeneous disease and patient selection is key to success. The indications for upfront cytoreductive nephrectomy remain for patients with single or oligometastatic disease who can be followed by observation. Patients who require systemic therapy should receive it first with the option to perform cytoreductive nephrectomy in case of symptoms or good response to therapy. Lastly, the decision-making process for metastatic RCC patients has become more complex, and should always be discussed in multidisciplinary tumor boards.
Presented by: Alessandro Volpe, MD, University of Eastern Piedmont Hospital, Maggiore Della Carita Hospital, Novara, Italy,
Written by: Hanan Goldberg, MD, Urology Department, SUNY Upstate Medical University, Syracuse, New-York, USA @GoldbergHanan at the 39th Congress of the Société Internationale d'Urologie, SIU 2019, #SIUWorld #SIU2019, October 17-20, 2019, Athens, Greece
References:
- Flanigan RC, Salmon SE, Blumenstein BA, et al. Nephrectomy Followed by Interferon Alfa-2b Compared with Interferon Alfa-2b Alone for Metastatic Renal-Cell Cancer. New England Journal of Medicine 2001; 345(23): 1655-9.
- Méjean A, Ravaud A, Thezenas S, et al. Sunitinib Alone or after Nephrectomy in Metastatic Renal-Cell Carcinoma. New England Journal of Medicine 2018; 379(5): 417-27.
- Bex A, Albiges L, Ljungberg B, et al. Updated European Association of Urology Guidelines for Cytoreductive Nephrectomy in Patients with Synchronous Metastatic Clear-cell Renal Cell Carcinoma. Eur Urol 2018; 74(6): 805-9.


