Athens, Greece (UroToday.com) Dr. Laurence Klotz initiated this session on prostate cancer screening. According to Dr. Klotz, there are several problems with the current paradigm with PSA and systematic biopsy:
- PSA thresholds are too confusing for primary care physicians with no consensus at sight
- Overdiagnosis of insignificant cancer is a real problem
- Pathologic miss of significant cancer and misattribution of grade
- Biopsy complications
- Discomfort as patients dislike biopsies
PSA with all its resulting controversy and the fact that different societies and organizations have conflicting recommendations regarding its use (Figure 1), is still here to stay. It has had a greater impact on cancer detection, staging, prognosis, and monitoring than any other biomarker had had in any cancer (Figure 2). It is more accessible, ubiquitous, quantitative, reproducible, and accurate than any other cancer biomarker. There is also compelling evidence regarding its role as a screening tool. An important factor to consider is the PSA level in midlife which can predict the lifetime risk of prostate cancer metastases/death with profound accuracy.
Figure 1 – PSA recommendation by various groups around the world: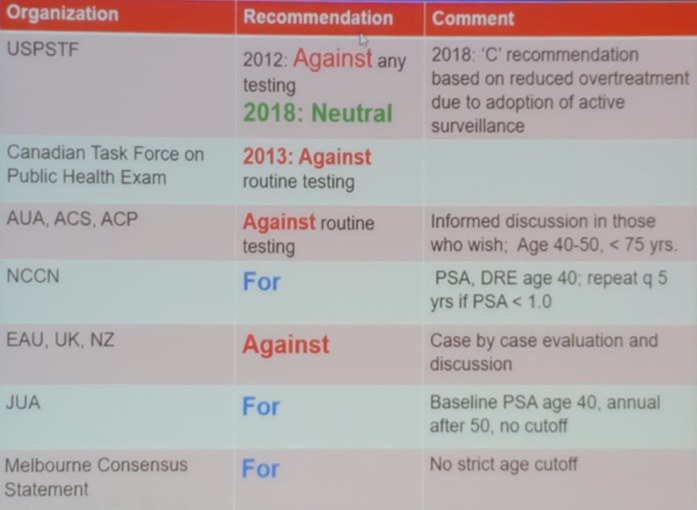
Figure 2 – Incidence of prostate and breast cancer metastatic diagnosis in the US 1975-2012: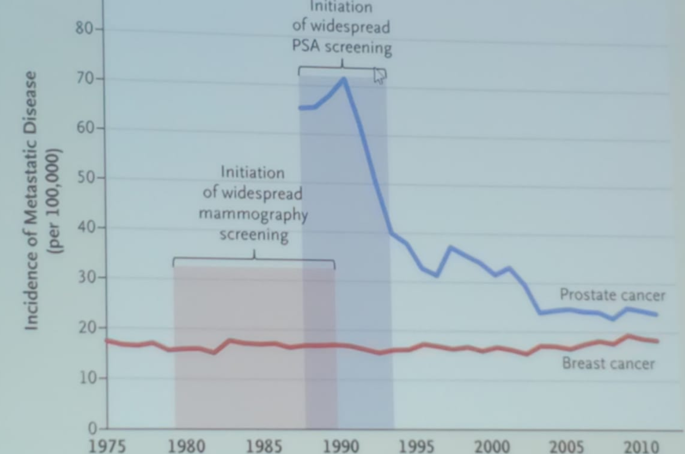
After the US preventative services task force (USPSTF) recommendation in 2012 against prostate cancer screening with PSA, data have shown a steady increase in the incidence of metastatic prostate cancer in the US (Figure 3).
Figure 3 – Increasing incidence of metastatic prostate cancer in the US (2004-2013):1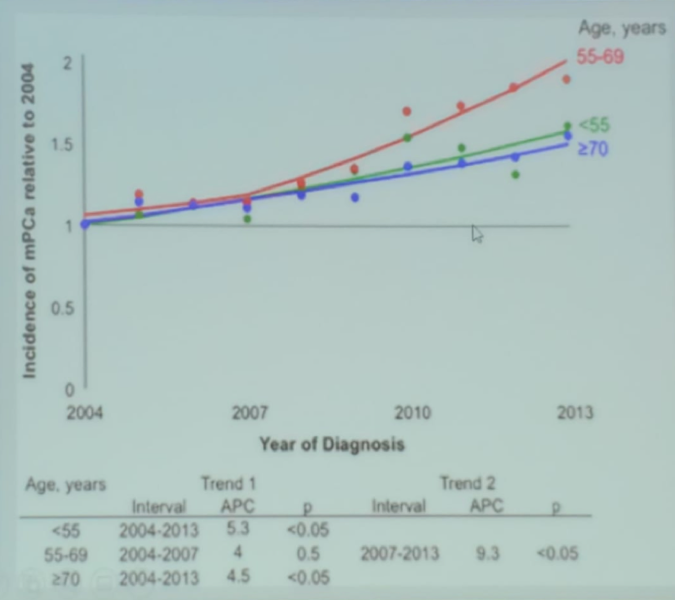
Clearly, the incidence of advanced prostate cancer disease at diagnosis is increasing since 2010. There is also no comparable improvement in countries without prevalent PSA testing. Properly performed large randomized trials show a 21-44% mortality reduction (29-56% among men screened) (Figure 4). The number need to screen with PSA is 293 per one death that can be avoided. The number needed to treat at 14 years is 12 (this is likely to even further decrease with longer follow-up). When comparing this to mammography, the number needed to screen is 111-235 at age 50-70, and the number needed to treat is between 10-14, and in colonoscopy, the number needed to screen is 850.
Figure 4- Results of the key prospective randomized screening trials: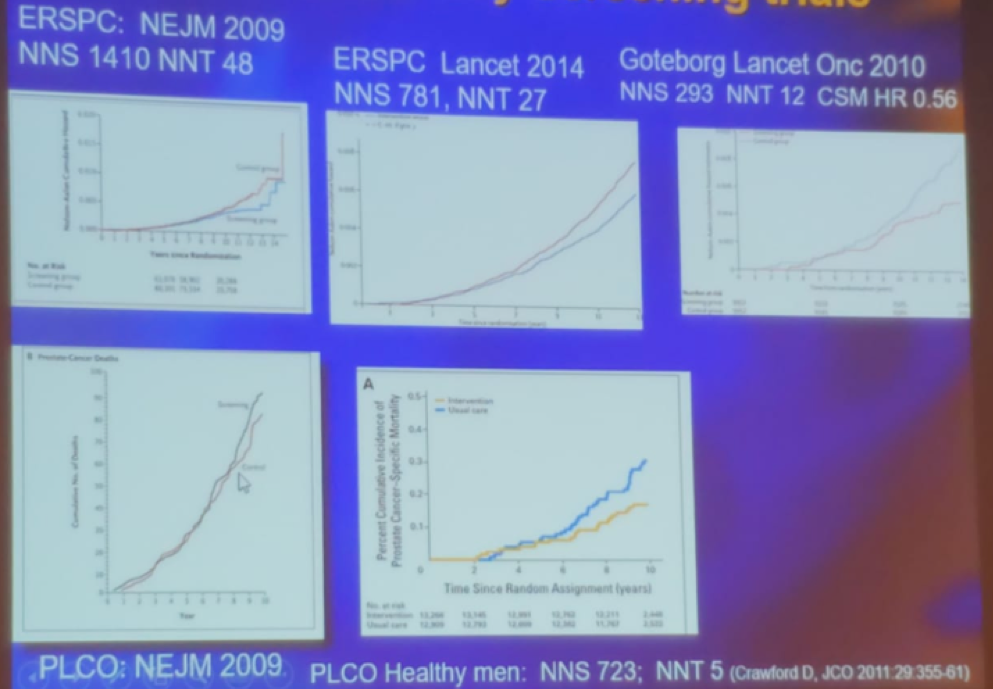
PSA done at midlife can predict the risk of metastases and prostate cancer-specific death. In a large study by Vickers et al. assessing 21,277 men aged 33-50, it was shown that the probability of metastases developing in 20-25 years in men with a PSA of less than 1.1 ng/ml is approximately 0.2%.2 Another important study by Halpern et al. evaluated the value of digital rectal examination (DRE) in the detection of significant prostate cancer.3 In a large cohort of 35,350 men in the screening arm of the PLCO study, it was shown that DRE made a difference only when the PSA level was above 3.0 ng/ml (23% vs. 13.7%). Thus the authors supported the restriction of DRE to men with PSA > 3.0 ng/ml as a reflex test to improve specificity.3
Dr. Klotz gave a possible solution to performing “informed PSA screening.” This entails:
- 1st test at ~age 45. If it is less than 1 then repeat every 5 years, with only 2-3 tests between the ages of 55-65.
- Screening above age 70 is probably not recommended.
- Incorporate additional blood/urine biomarkers
- Utilization of active surveillance for most low-risk disease
- There is an emerging role for MRI to perhaps replace the biopsy at specific settings
Another option is to use a lower PSA cutoff of 1.5 ng/ml as has been suggested by Dr. Crawford4 (Figure 5).
Dr. Klotz moved on to describe what the available options are when faced with an elevated PSA. This is basically choosing between performing a multiparametric MRI and using another biomarker. Table 1 demonstrates the differences between these two options. The problem with newly found biomarkers is the cost and the analytical expertise that is required for their interpretation5 (Figure 6).
Dr. Klotz concluded his talk suggesting rehabilitation for PSA testing. The patient needs good information which is difficult for the physician to convey in the typical average clinic visit. That is why a good patient brochure is required. It is important to restrict testing to those who will benefit and restrict the biopsy to those with a compelling reason. Active surveillance should be utilized for low-risk patients. Lastly, the treatment morbidity should be reduced by treating patients at centers of excellence and exploring the option of focal therapy for properly selected patients.
Figure 5: Approach to shared care in prostate cancer diagnosis using a PSA cutoff of 1.5 ng/ml:4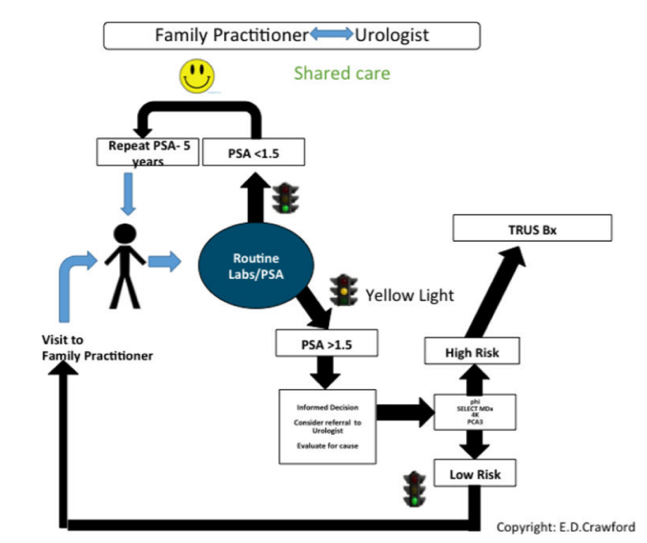
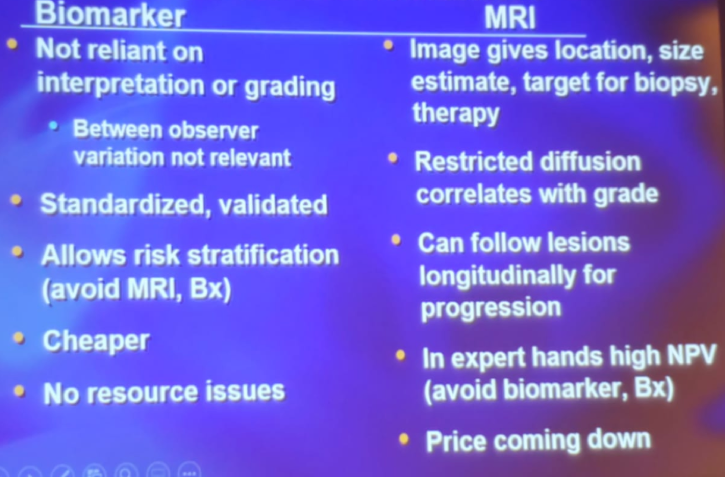
Table 1 – Multiparametric MRI or biomarker? What to use when faced with an elevated PSA?
Figure 6 – The cost and complexity of liquid biomarker diagnostics: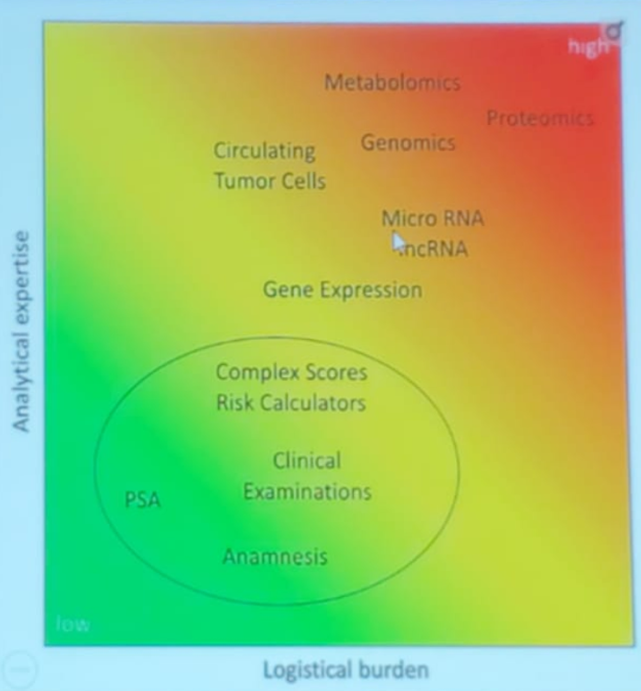
Presented by: Laurence Klotz, MD, FRCSC, Professor, Department of Surgery, University of Toronto, Toronto, Canada
Written by: Hanan Goldberg, MD, Urology Department, SUNY Upstate Medical University, Syracuse, New-York, USA @GoldbergHanan at the 39th Congress of the Société Internationale d'Urologie, SIU 2019, #SIUWorld #SIU2019, October 17-20, 2019, Athens, Greece
References:
- Weiner AB, Matulewicz RS, Eggener SE, Schaeffer EM. Increasing incidence of metastatic prostate cancer in the United States (2004-2013). Prostate cancer and prostatic diseases 2016; 19(4): 395-7.
- Vickers AJ, Ulmert D, Sjoberg DD, et al. Strategy for detection of prostate cancer based on relation between prostate specific antigen at age 40-55 and long term risk of metastasis: case-control study. BMJ : British Medical Journal 2013; 346: f2023.
- Halpern JA, Oromendia C, Shoag JE, et al. Use of Digital Rectal Examination as an Adjunct to Prostate Specific Antigen in the Detection of Clinically Significant Prostate Cancer. The Journal of urology 2018; 199(4): 947-53.
- Crawford ED, Rosenberg MT, Partin AW, et al. An Approach Using PSA Levels of 1.5 ng/mL as the Cutoff for Prostate Cancer Screening in Primary Care. Urology 2016; 96: 116-20.
- Neuhaus J, Yang B. Liquid Biopsy Potential Biomarkers in Prostate Cancer. Diagnostics (Basel) 2018; 8(4): 68.


