Athens, Greece (UroToday.com) Dr. Georg Salomon presented the novel multiparametric ultrasound for prostate cancer detection and localization, and its correlation to ultrasound B mode, shear wave elastography, and contrast-enhanced ultrasound with radical prostatectomy specimens.
Multiparametric MRI (mpMRI) is superior to systematic biopsies with fewer cores, and lower detection rate of insignificant cancer1. However, it has some limitations which include but not limited to missing significant cancer, and importantly it is not a urologic procedure, performed almost entirely by radiologists.
According to Dr. Salomon that is where the multiparametric ultrasound can fill the gap. It is a potential method, which is as good as mpMRI (or perhaps even better), cheaper and faster than mpMRI, and performed by a urologist and not a radiologist. The currently used conventional ultrasound is not multiparametric.
When comparing the various modalities of ultrasound to whole-mount pathology sections the sensitivities and specificities can be seen in table 1.
Table 1 – Comparison of ultrasound to whole-mount pathologic sections: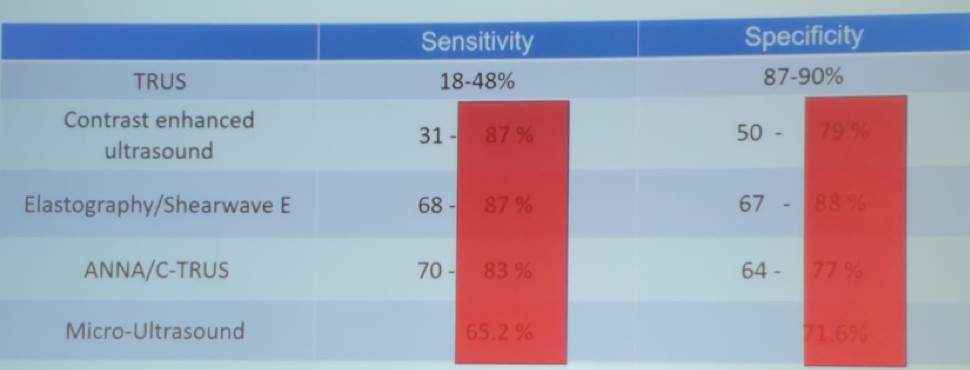
The main advantages of ultrasound include:
- Practical, fast and cheap
- Well-known and used frequently by urologists
- Enables to perform a real-time biopsy
- Easy to integrate into the workflow
The idea behind the multiparametric ultrasound is to develop an ultrasound-based algorithm or scoring system combining all its various parameters (multiparametric classifier) into one test (Figure 2).
Figure 2 – The various ultrasound parameters: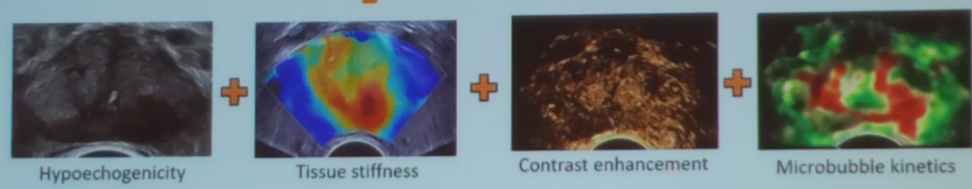
The multiparametric ultrasound study was an investigator-initiated prospective single-center study (NCT03091231) including 50 men scheduled for radical prostatectomy. The inclusion and exclusion criteria are shown in Table 2.
Table 2 – Inclusion and exclusion criteria in the multiparametric ultrasound study:
All patients underwent imaging of three planes, with B-mode, shockwave elastography (SWE), and contrast-enhanced ultrasound (CEUS). The imaging results were matched to histopathologic specimens. The primary outcome was the diagnosis of clinically significant cancer, defined as a region of interest with:
- Gleason score of 3+4 or above
- A tumor volume >=0.5 ml
- Extracapsular extension
More stringent definitions were included as well. A result was regarded as positive if the region of interest contained the index of prostate cancer lesion.
The sensitivity and negative predictive value for clinically significant prostate cancer for a lesion with a Likert>=3 is shown in Table 3.
Table 3 – Sensitivity and negative predictive value of a lesion at Likert >=3: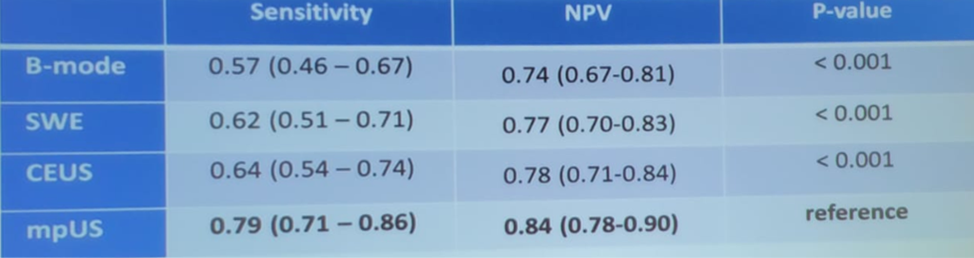
In conclusion, the multiparametric ultrasound appears to be safe and feasible and can be performed in less than 30 minutes with good imaging quality. It significantly improved the sensitivity of clinically significant prostate cancer localization. It demonstrated high ability to detect the index lesion compared with individual conventional ultrasound modalities. With more data coming in and being validated, the multiparametric ultrasound could serve as a serious contender to replace mpMRI in the future.
Presented by: Georg Salomon, MD, PhD, University of Hamburg, Martini-clinic, Hamburg, Germany
Written by: Hanan Goldberg, MD, Urology Department, SUNY Upstate Medical University, Syracuse, New York, USA, Twitter: @GoldbergHanan at the 39th Congress of the Société Internationale d'Urologie, SIU 2019, #SIUWorld #SIU2019, October 17-20, 2019, Athens, Greece
References:


