Athens, Greece (UroToday.com) Dr. Derya Tilki was the first to present at the Educating Masterclass on Biochemical Recurrence after Radical Prostatectomy. Her talk focused on the long-term outcomes of patients with biochemical recurrence (BCR) after radical prostatectomy.
Following radical prostatectomy, approximately 27-53% of patients will experience BCR.1 However, only 30% of patients experiencing BCR after primary surgery will develop clinical recurrence, with only 16.4% dying from their disease. The main unfavorable prognostic factors are:
- PSA doubling time (PSADT) of <=1 year
- A pathological Gleason score 8-10.1
According to the EAU guidelines, there are low risk and high BCR definitions stratified by primary treatment, as seen in table 1. High-risk BCR patients have been shown to have significantly better survival when salvage radiotherapy (SRT) was delivered at an early stage (PSA<0.5 ng/ml) compared with no SRT. In contrast, in low-risk BCR patients there was no protective effect of early SRT.2
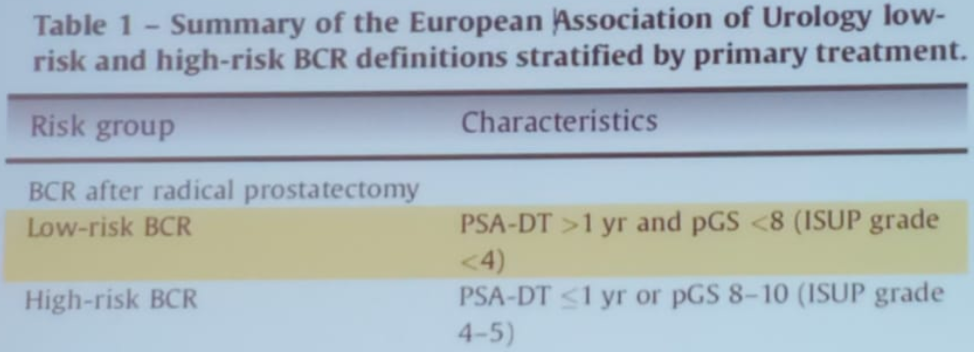
Table 1 – Low and high-risk biochemical recurrence definitions according to the EAU:
Next, Dr. Tilki discussed the significance of persistent PSA following radical prostatectomy. Between 5-20% of men continue to have detectable persistent PSA after radical prostatectomy (>0.1 ng/ml), within 4-8 weeks of surgery. There are several possible reasons for this increased PSA:
- Persistent local disease
- Pre-existing metastases
- Residual benign prostate tissue
In a large study including more than 11,000 men after radical prostatectomy, the authors assessed the impact of persistent PSA on outcomes. Out of the 11,604 men after radical prostatectomy, 8.8% demonstrated persistent PSA.3 At 15-year follow-up, metastases free survival (MFS) and cancer specific survival (CSS) were 53% vs. 93.2% (p<0.01) and 75.5% vs. 96.2% (p<0.001), respectively, for persistent vs. undetectable postoperative PSA (Figure 1). In multivariable analyses, the following were associated with an increased risk for persistent PSA (all p<0.01):
- Higher preoperative PSA
- More advanced pathologic tumor stage
- Pathologic Gleason group 3-5
- Positive surgical margins
- Pathological stage N1
Figure 1 - Metastasis free survival and cancer specific survival in men with persistent PSA compared to undetectable postoperative PSA:
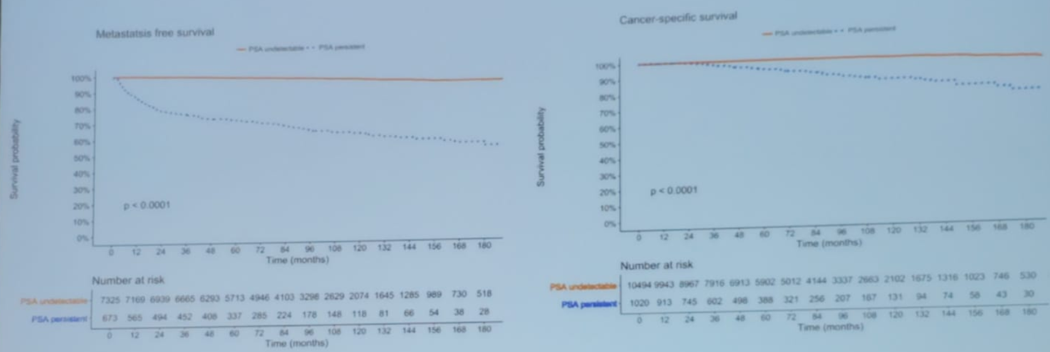
In propensity score matching between patients who received SRT vs. no SRT, the CSS at 10 years after radical prostatectomy was 93.7% vs. 81.6% in the entire cohort (p<0.01). However, in a sub-analysis including only patients with pathological N1 disease, the CSS was 96.2% for those who received SRT compared to 55.8% in patients who did not receive SRT.3
Due to these findings of persistent PSA, the EAU guidelines have added in their most recent guidelines recommendations regarding the management of persistent PSA after radical prostatectomy. These include performing PSMA PET in men with persistent PSA (>0.2 ng/ml) to exclude metastatic disease and treating men with no evidence of metastatic disease with SRT and hormonal therapy (Table 1).
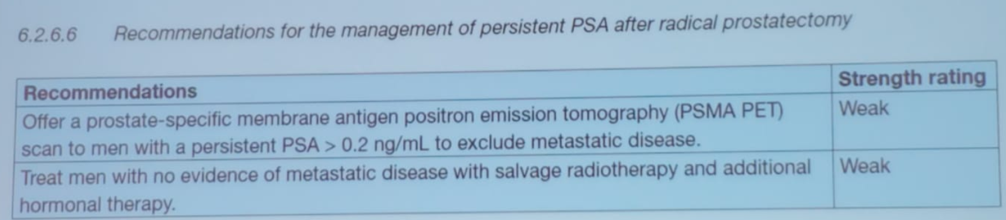
Table 1 – EAU recommendations for the management of persistent PSA after radical prostatectomy:
Dr. Tilki concluded her talk stating that PSA recurrence has several definitions. The new EAU guidelines have shifted from absolute value to risk groups (low and high). Not all BCR progress to clinical recurrences or cancer death. Lastly, persistent PSA after radical prostatectomy is associated with more advanced disease and poor prognosis. The available data suggests that patients with PSA persistence may benefit from early aggressive multi-modality treatment.
Presented by: Derya Tilki, MD, Attending Urologist at the Martini-Klinik Prostate Cancer Center, University Hospital Hamburg-Eppendorf in Hamburg, Germany
Written by: Hanan Goldberg, MD, Urology Department, SUNY Upstate Medical University, Syracuse, New-York, USA @GoldbergHanan at the 39th Congress of the Société Internationale d'Urologie, SIU 2019, #SIUWorld #SIU2019, October 17-20, 2019, Athens, Greece
References:
- Van den Broeck T, van den Bergh RCN, Arfi N, et al. Prognostic Value of Biochemical Recurrence Following Treatment with Curative Intent for Prostate Cancer: A Systematic Review. Eur Urol 2019; 75(6): 967-87.
- Tilki D, Preisser F, Graefen M, Huland H, Pompe RS. External Validation of the European Association of Urology Biochemical Recurrence Risk Groups to Predict Metastasis and Mortality After Radical Prostatectomy in a European Cohort. Eur Urol 2019; 75(6): 896-900.
- Preisser F, Chun FKH, Pompe RS, et al. Persistent Prostate-Specific Antigen After Radical Prostatectomy and Its Impact on Oncologic Outcomes. Eur Urol 2019; 76(1): 106-14.


