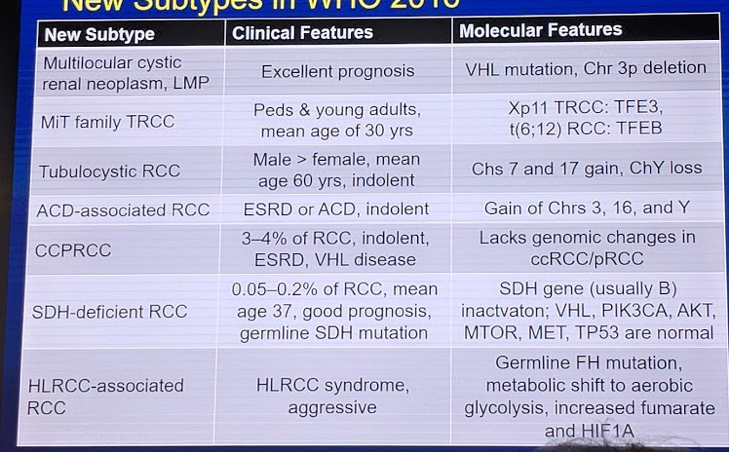
Adapted from Inamura et al. (Int J. Mol Science): New WHO subtypes introduced in 2016
We know from multiple studies now, including work by Dr. Leibovich’s group at the Mayo Clinic (J Urol 2010), that histology alone is a predictor of cancer-specific survival – ccRCC, when matched for stage, grade, and necrosis, had a 2-fold increased risk of CSM than chromophobe and papillary RCC.
In this talk, he focused on different hereditary syndromes as these have provided a lot of knowledge regarding the genetics/genomics of even sporadic RCC.
- Shuch et al. (JCO 2014) – found that using age 46 could help separate patients with familial syndromes vs. sporadic RCC relatively well. Bell curve for patients with syndromic RCC falls below this age cutoff, while most sporadic RCC develops after.
- Leibovich uses this age cutoff as well – patients diagnosed before age 46 or with other symptoms/sequelae of syndromes should be tested
- VHL and clear cell RCC
- Due to 3p25- (VHL gene), which is a tumor suppressor gene
- Penetrance
- 75% of VHL patients have ccRCC
- But, only 1.6% of all ccRCC patients have VHL
- *~90% of sporadic ccRCC have some alteration of the VHL gene though
- Prognostic impact – conflicting data
- Current understanding is that it doesn’t impact treatment or prognosis
2. Hereditary papillary RCC
- -Due to 7q31- cMET oncogene mutation
- - This is also strongly expressed in many sporadic types 1 and type 2 papillary RCC
- papillary RCC is the ONLY manifestation – usually bilateral multifocal papillary type I tumors
- Therapy – targeted therapy against MET (foratenib) showed good promise in a phase II trial (Choueri et al. JCO 2013)
- Prognostic – Sweeney et al. demonstrated that c-met (+) patients had much worse OS
- Hereditary Leiomyomatosis and RCC syndrome (HLRCC)
- Genetic mutation: fumarate hydratase (FH) 1q42, probably tumor suppressor
- These mutations are uncommon in sporadic RCC
- Birt-Hogg-Dube (BHD)
- Genetic mutation: folliculin (17p11.2) – function not clear, but likely plays a role in mTOR complex regulation
- Uncommon in sporadic RCC
He did note that if you have an interest in the genomic landscape of RCC, a must-read article is the following: Rickets CJ et al. “TCGA Molecular characterization of RCC” in Cell Reports.
- 843 RCC cases – mostly ccRCC (488) and papillary RCC (270)
- Confirmed prior reports that histology associated with survival differences
- Genetic changes consistent with prior knowledge – but also add much more details and other genetic changes not previously known
- 16 significantly mutated genes in RCC (9 in ccRCC, 11 in pRCC, 2 in chRCC)
- Chromatin remodeling gene mutations varied by histologic subtype – with variable impact on survival
- Specifically pointed out BAP1 and PBRM1 mutations
- Germline BAP1 mutations associated with RCC … and uveal/skin melanomas and pleural malignant mesotheliomas. Rare, but will need to work with ortho oncology and thoracic oncology colleagues.
- Metabolic gene expression profiles were also associated with different histologic subtypes
- Patients with multiple metabolic gene defects had much worse survival, even within a single histology
- Immune cell gene signature analysis demonstrated almost universal upregulation in ccRCC compared to other histologic subtypes
- ClearCode 34 is a genetic signature that was developed to separate patients into clear cell A (ccA) and ccB subtypes
- Subtype has clear associations with survival outcomes – ccB had worse RCC-specific survival than ccA (Serie et al. EU 2016)
- Interestingly, when comparing primary to metastases, while ccB primaries often led to ccB mets, ccA primaries often also led to ccB mets!
Presented by: Bradley Leibovich, MD, Urologist, Chair, Mayo Clinic, Minnesota, United States
Written by: Thenappan Chandrasekar, MD, Clinical Instructor, Thomas Jefferson University at the 38th Congress of the Society of International Urology - October 4- 7, 2018 - Seoul, South Korea


