(UroToday.com) The 2022 Southeastern Section of the AUA’s annual meeting included a bladder cancer session and Dr. Bryce Baird discussing the association between visibly complete TURBT and pathologic downstaging following neoadjuvant chemotherapy and radical cystectomy for muscle-invasive bladder cancer. Neoadjuvant chemotherapy followed by radical cystectomy is a standard of care in patients with muscle-invasive bladder cancer. However, there are conflicting data regarding the potential oncologic benefit of a visibly complete TURBT prior to neoadjuvant chemotherapy and radical cystectomy. Furthermore, the improved local staging offered by bladder MRI has called into question the value of a TURBT prior to neoadjuvant chemotherapy for patients with imaging evidence of muscle-invasive tumors. The primary aim of this study was to evaluate if a visibly complete TURBT is associated with pathologic outcomes after neoadjuvant chemotherapy and radical cystectomy.
This study included a retrospective review of an institutional radical cystectomy database from 2011 to 2021 to identify patients who received neoadjuvant chemotherapy and radical cystectomy for muscle-invasive bladder cancer. Records were independently reviewed to assess the completeness of TURBT. Six patients with missing TURBT data were classified as having an incomplete resection. The primary outcome was pathologic downstaging, defined as <pT2 at radical cystectomy, and secondary outcomes included pT0 rate, as well as overall, cancer-specific, and recurrence-free survival.
A total of 158 patients were identified, including 119 (75%) with a visibly complete TURBT; there were no significant differences in baseline characteristics between patients receiving complete versus incomplete TURBT. Additionally, there was no significant difference in the rate of pathological downstaging for those with (42%) and without (34%) a visibly complete TURBT, (p = 0.39). Similarly, there was no significant difference in the rate of complete pathologic response at radical cystectomy between those with (30%) and without (26%) a visibly complete TURBT (p = 0.64). After adjusting for age, gender, preoperative hydronephrosis, ECOG status, type of chemotherapy and time from last chemotherapy to radical cystectomy, there was no significant association between visibly complete TURBT and pathologic downstaging (adjusted OR 0.92, 95% CI 0.39-2.20) or compete pathologic response (OR 0.77, 95% CI 0.30-2.00). According to TURBT status, patients with a complete TURBT versus an incomplete TURBT had improved survival:
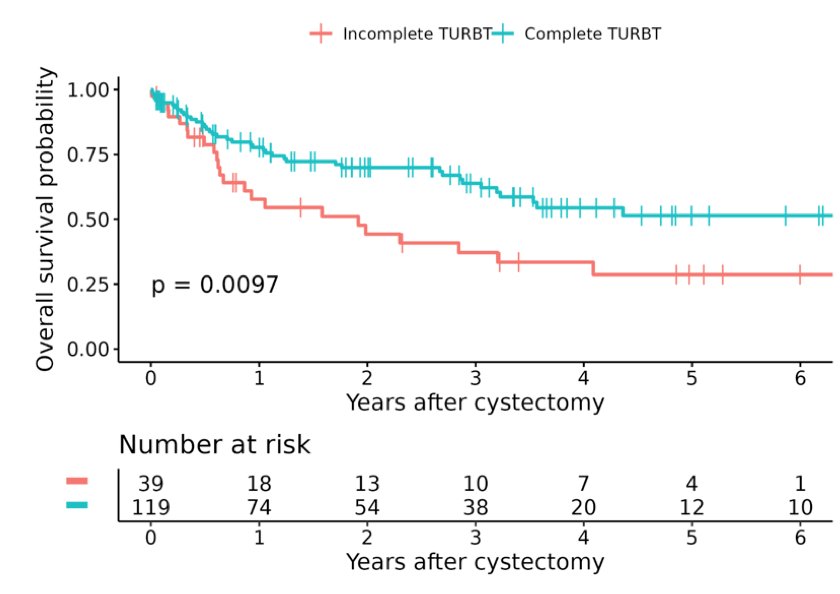
However, there was no difference in recurrence-free survival (p = 0.21) or cancer-specific survival (p = 0.068).
Dr. Baird concluded his presentation assessing the role of complete versus incomplete TURBT on outcomes after neoadjuvant chemotherapy and radical cystectomy with the following take-home messages:
- A visibly complete TURBT was not associated with pathologic response following neoadjuvant chemotherapy and radical cystectomy
- Overall survival was better in the complete TURBT group, with no difference in recurrence-free survival or cancer-specific survival
- These data do not support the need for a repeat TURBT to achieve a visibly complete resection of a muscle-invasive tumor if neoadjuvant chemotherapy and radical cystectomy are planned
- We await data from the ongoing randomized phase II/III BladderPath study
Presented By: Bryce Baird, MD, Mayo Clinic Florida, Department of Urology, Jacksonville, FL Co-Authors: Augustus Anderson, MD2, Christian Ericson, MD1, Gianpiero Carames3, Colleen Ball, MS3, Paul Young, MD1, Timothy Lyon, MD1 Affiliations: 1Mayo Clinic Florida, Dept of Urology, 2Tulane School of Medicine, 3Mayo Clinic Florida
Written By: Zachary Klaassen, MD, MSc – Urologic Oncologist, Assistant Professor of Urology, Georgia Cancer Center, Augusta University/Medical College of Georgia, @zklaassen_md on Twitter during the 86th Annual Meeting of the Southeastern Section of the American Urological Association, San Juan, PR, Mar 16 – 19, 2022


