Figure 1- Prostate cancer diagnosed by an autopsy by race:

There are available calculators, such as the European Randomized study of Screening for Prostate Cancer (ERSPC) risk calculator that provide the risk of prostate cancer, even without the value of a PSA test. The Rotterdam ESPEC risk calculators can be found online and provide an estimated risk of having a positive prostate biopsy.
The European Association of Urology (EAU) guidelines recommend offering to screen for prostate cancer to well-informed men, after counseling them about the potential risks and benefits. In any case, a single elevated PSA should not prompt immediate biopsy. PSA should be verified after a few weeks in second testing before performing a biopsy. The past habit of providing empiric antibiotics in an asymptomatic patient to lower the PSA should not be undertaken.
There has been much discussion and debate on the appropriate cut off value of PSA, and at what PSA value to refer a patient for a prostate biopsy. The classic cut off 3.1-4 ng/ml harbors a 26.9% risk of any prostate cancer, and a 6.7% risk of clinically significant prostate cancer (Gleason score 3+4=7), based on the Prostate Cancer Prevention Trial (PCPT)1. The PCPT risk calculator can also be found online.
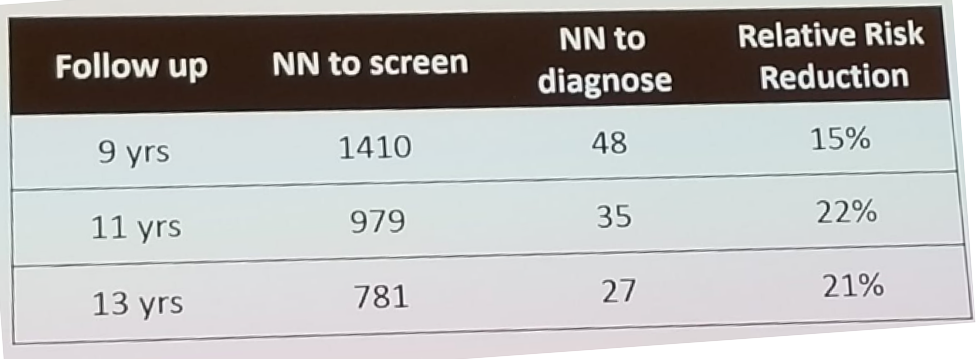
When looking at the results of the ERSPC study at 9,11, and 13 years follow-up (Table 1) it is possible to see that with extended follow-up, the mortality relative risk reduction remains unchanged. However, the number needed to screen and to diagnose is decreasing rapidly (below the number needed to screen in breast cancer trials). Screening has both advantages and disadvantages. The befits include the reduction of prostate cancer-specific mortality and metastases. The disadvantages include the overdiagnosis of low-grade tumors and overtreatment of these tumors.
Table 1- Key findings from the ERSPC study at long-term follow-up:
Next, the speakers debated which patients die from prostate cancer. Figure 2 demonstrates the natural evolution of non-curatively treated prostate cancer in comparison to cardiovascular death and other cause mortality. 2 As demonstrated by the figure, 10%, 20%, and 40% of patients with low-, intermediate-, and high-risk prostate cancer, respectively, die of prostate cancer.
Figure 2- the Natural evolution of non-curatively treated prostate cancer patients:

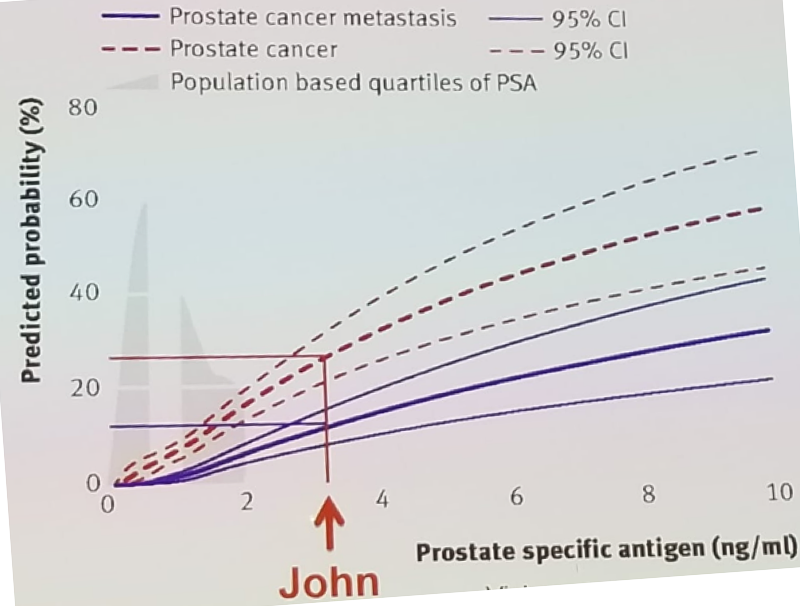
The problem of overdiagnosis and overtreatment of non-aggressive low-risk indolent disease is a real issue and needs to be addressed. A study published by Vickers A et al. demonstrated that a first PSA at the age of 45-49 could predict which men would die of prostate cancer in the future3. The results demonstrated that 10% of men with the highest PSA (above 1.5 ng/ml) are responsible for 44% of prostate cancer deaths in the future. Another study published by Vickers A. et al.4 showed that PSA at the age of 60 could be correlated to the lifetime risk of prostate cancer or prostate cancer metastases. For example, figure 3 demonstrates a 60-year-old man with a PSA of 3 ng/ml, having a 30% lifetime risk of prostate cancer and a 15% lifetime risk of prostate cancer metastases. The Rotterdam ERSPC risk calculators mentioned earlier, allow us to incorporate the PSA value, the digital rectal examination result, prior negative prostate biopsy, and the prostate volume, to give a more accurate risk of positive prostate biopsy and more specifically, the risk of high-grade prostate cancer. A result of less than 12.5% should not mandate a biopsy, 12.5%-20% - should mandate a biopsy only if the risk of high-risk cancer is >4%, and above 20% must mandate a biopsy.
Figure 3 – Lifetime risk of clinically diagnosed prostate cancer and prostate cancer metastases based on PSA at age 60:
Over the years, there has been an increasing number of tests on the market developed to help us choose which patients we need to refer for a prostate biopsy. These include the urine PCA3 test, the Prostatic Health Index (PHI), the SelectMDx test, and the 4Kscore test. The PCA3-RNA test is based on a pseudogene that, if transcribed, generates a non-coding RNA. It is selectively expressed in the prostate and is overexpressed in prostate cancer. The PHI test gives us a number resulting from an equation composed of [-2]proPSA + free PSA + total PSA. The PHI has an area under the curve (AUC) of 0.7-0.77, with a negative predictive value of 67-92%, a risk of missing prostate cancer between 8-33%, and resulting in 36% of unnecessary biopsies that could be avoided. SelectMDX, similarly to the PCA3 test, is based on mRNA biomarker isolated from the urine. The presence of HOXC6 and DLX1 mRNA levels are assessed to provide an estimate of the risk of prostate cancer in general, and high-risk prostate cancer specifically. It has an AUC of 0.9, with a negative predictive value of 98%, with a 2% risk of missing high-grade prostate cancer, and it can avoid 53% of unnecessary prostate biopsies. A more newly found test is the 4Kscore, which combines four prostate-specific kallikrein assay results with clinical information in an algorithm that calculates the individual patient’s percent risk for aggressive prostate cancer. It has an AUC of 0.82, a negative predictive value of 95%, a 5% risk of missing prostate cancer, and can avoid 36% of unnecessary biopsies.
Dr. Joiniau concluded his encompassing discussion and showed the recommendations of the EAU guidelines on PSA testing. According to the guidelines PSA should be offered to well-informed men at elevated risk of prostate cancer. These include men above the age of 50, men above the age of 45 with a family history of prostate cancer, or men older than 45 who are African-American. For men who have had an initial PSA level, we should retest them in two years-time if they have a PSA above one ng/ml at the age of 40, or above two ng/ml at the age of 60. Men with lower PSA values should be followed up in eight years time. Men who have a life expectancy of <15 years are unlikely to benefit from PSA testing. Lastly, table 2 summarized the recommendations for PSA testing in men aged 50-70 according to the EAU guidelines.
Table 2 – PSA testing recommendations according to the EAU guidelines:

Presented by: Mark Emberton, London, Great Britain and Steven Joniau, Leuven, Belgium
Written by: Hanan Goldberg, MD, Urologic Oncology Fellow (SUO), University of Toronto, Princess Margaret Cancer Centre, Twitter:@GoldbergHanan at the 2nd EAU Update on Prostate Cancer (PCa18)– September 14-15, 2018 – Milan, Italy
References:
1. Thompson IM et al. NEJM 350 (22):2239-46, 2004
2. Rider JR et al. Eur Urol 2012
3. Vickers A et al. BMJ 2013
4. Vickers A et al. BMJ 2010; 341


