(UroToday.com) The International Kidney Cancer Symposium 2021 annual hybrid meeting included a non-clear cell renal cell carcinoma (RCC) session and a presentation by Dr. Ronald Boris discussing surgical management of non-clear cell renal cell carcinoma (RCC). Dr. Boris notes that histology matters in the behavior of both local and advanced RCC. Histology may allow us to better define what a small renal mass is, for example a chromophobe RCC may be “small” (ie. behave as a small renal mass) when up to 8 cm in size. Papillary RCC is more likely to demonstrate worse prognosis for T3b/T3c disease and have a higher predilection for lymph node involvement. Generally, clear cell papillary and papillary RCC show the highest level of local recurrence, especially in advanced stages, while papillary and unclassified RCC have the worst survival. Not surprisingly, collecting duct and sarcomatoid differentiation demonstrate the highest metastatic rates among all histologies.
Dr. Boris emphasized that many of the nuances of partial nephrectomy and renal tumor surgery evolved from the hereditary RCC experience. More specifically, renal tumor enucleation or parenchymal sparing surgery was “created” for patients with genetic predisposition to bilateral multifocal renal masses. The initial tenets for surgery in these patients focused on tumor removal (with little regard for margin), renal parenchyma preservation, and limiting hilar ischemia. However, recently these surgical strategies (ie. tumor enucleation) have been applied to sporadic RCC management with encouraging results. In a European collaborative report,1 332 patients underwent tumor enucleation, compared to 143 patients undergoing radical nephrectomy, with no difference in 5- and 10-year progression free survival between the groups (95% and 93% for tumor enucleation versus 91% and 88% for radical nephrectomy). As such, surgical technique did not predict progression-free or cancer-specific survival.
One of the observations Dr. Boris had while working at the NIH was that tumors associated with different syndromes followed specific intra-operative patterns (ie. VHL versus BHD versus HPRC, etc). Could the tumor pseudocapsule explain these findings? A tumor pseudocapsule separates most renal tumors from adjacent parenchyma, and tumors can be shelled out ‘perfectly’ (ie. enucleation) or modified as a hybrid resection. The hypothesis is that the pseudocapsule may impact the ability to remove and handle these tumors safely during a partial nephrectomy. Work from Dr. Boris’ group assessed peritumoral pseudocapsules of 160 pT1 renal tumors, including 60 clear cell RCCs, 50 papillary RCCs, 25 chromophobe RCCs, and 25 oncocytoma. They found that a complete pseudocapsule was found in 77% of clear cell tumors, 74% of papillary, 28% of chromophobe, and 4% of oncocytomas. Tumor pseudocapsule was present but incomplete in 18% of clear cell, 18% of papillary, 44% of chromophobe, and 56% of oncocytoma. Ultimately, clear cell RCC shows the most consistent pseudocapsule (and is the best candidate for enucleation), with a lower rate of invasion beyond it compared to papillary RCC, whereas chromophobe and oncocytoma characteristically have an incomplete or absent pseudocapsule. As follows is a representative example of a complete robust pseudocapsule in clear cell RCC (a) and complete invasion into surrounding parenchyma for papillary RCC (b):
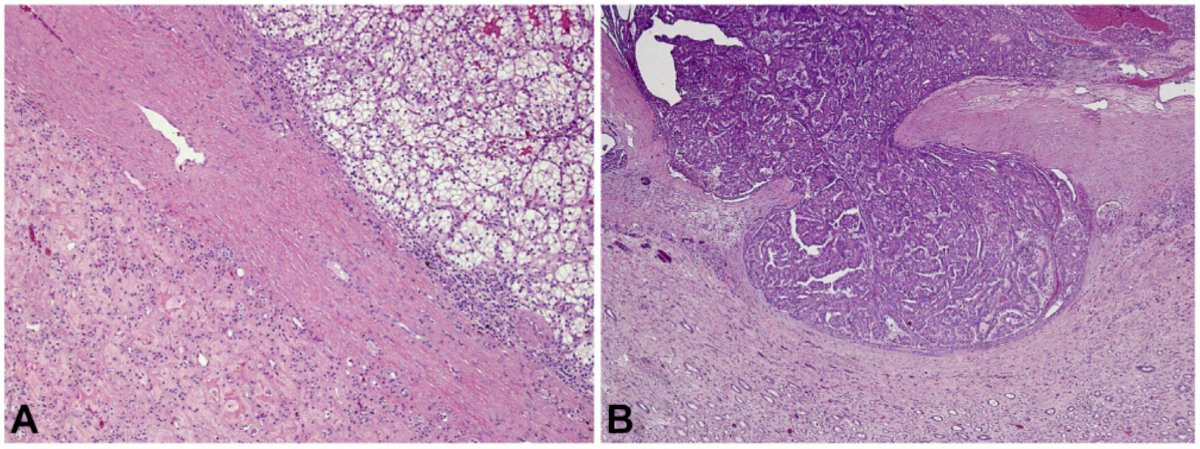
This work was subsequently validated by Xi et al.,3 noting that the status of the tumor pseudocapsule has prognostic implications for RCC, and that complete pseudocapsule positively improves overall survival. A lack of a pseudocapsule is major adverse risk factor, and thus reporting and understanding the pseudocapsule status is an important parameter in clinical practice.
Moving to surgery beyond the localized renal mass, there is an evolving role of cytoreductive nephrectomy in patients with metastatic RCC of variant histology. A recent review assessing this topic4 suggests the following:
- Targeted therapy results in inferior outcomes in non-clear cell mRCC compared to clear cell mRCC
- Population-based data from IMDC and SEER databases suggest that cytoreductive nephrectomy provides a survival benefit in non-clear cell mRCC patients, perhaps because of the lower response to targeted therapies compared with clear cell mRCC
- Level 1 evidence from CARMENA5 and other trials did not include non-clear cell histologies
- Recent trials with checkpoint inhibitors in mRCC prior to cytoreductive nephrectomy have also excluded patients with non-clear cell histology
Dr. Boris notes that metastasectomy is an acceptable treatment option for patients with metastatic RCC, and that in select patients (ie. good risk and intermediate-risk groups) surgery may yield long-term disease-free survival. The benefit of complete resection, even with multiple sites of disease, may result in a survival benefit of up to 3 years.
Taken together, Dr. Boris emphasized that a new approach to surgical management of kidney cancer is to understand the disease biology and characteristics unique to each subtype:
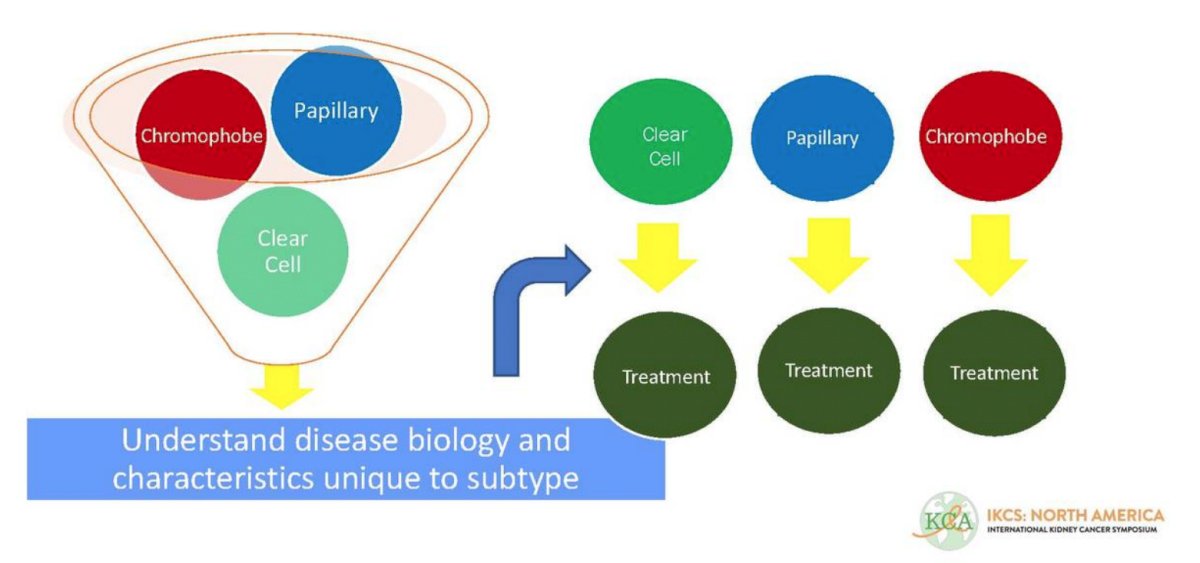
Pre-treatment tumor subtype acquisition may include a (i) renal mass biopsy, (ii) novel radiography (ie. CA-IX or other surface antigen-binding PET scans), (iii) liquid biopsy (blood or urine testing), and (iv) germline test for hereditary RCC. These diagnostic modalities are important for distinguishing low-grade from high-grade tumors, planning the surgical approach (ie. high-grade T3, consider radical nephrectomy/lymph node dissection), and assessing metastatic status. Dr. Boris’ summary of histology-specific management of RCC is as follows:
- Clear cell RCC:
- Low grade has high survival rates
- Excellent for enucleation
- Cytoreductive nephrectomy for metastasis should be considered
- Papillary RCC:
- Higher multifocality and local recurrence rate (especially for clear cell-papillary RCC)
- Poorer enucleation secondary to worse capsule invasion
- High grade tumors should have consideration for lymphadenectomy
- Cytoreductive nephrectomy for metastasis may be considered
- Chromophobe RCC:
- The “small renal mass” definition should be extended to 8cm
- Enucleation is harder but there is usually minimal invasion
- These tumors have an indolent behavior and are good candidates for active surveillance
- Cytoreductive nephrectomy for metastasis may be considered
Dr. Boris concluded his presentation with the following take-home messages:
- Understanding renal tumor subtyping and specific behaviors associated with RCC histology can shape surgical approaches in both the localized and metastatic settings
- Tumor enucleation, once applied in only cases of multifocal hereditary RCC, can be used best in the sporadic setting after understanding tumor and tumor pseudocapsule behavior and nuances
- For these reasons, continued efforts to easily obtain pre-treatment information (ie. histology grade, invasiveness) with novel imaging, biopsy, and genomic testing is warranted
- A “see tumor, remove tumor” approach for all renal masses may be shortsighted and ultimately creating a nuanced algorithm for surgical timing (active surveillance), extent (partial nephrectomy, radical nephrectomy, lymph node dissection), and utility for cytoreduction or metastatic resection will be best
Presented by: Ronald S. Boris, MD, MS, Assistant Professor of Surgery, Association Profession of Urology, Department of Urology, Indiana University, Indianapolis, GA
Written by: Zachary Klaassen, MD, MSc – Urologic Oncologist, Assistant Professor of Urology, Georgia Cancer Center, Augusta University/Medical College of Georgia, @zklaassen_md on Twitter during the International Kidney Cancer Symposium (IKCS) 2021 Annual Congress, November 5 and 6, 2021.
References:
- Minervini A, Serni S, Tuccio A, et al. Simple enucleation versus radical nephrectomy in the treatment of pT1a and pT1b renal cell carcinoma. Ann Surg Oncol. 2012;19:694-700.
- Jacob JM, Williamson SR, Gondim DD, et al. Characteristics of the peritumoral pseudocapsule vary predictably with histologic subtype of T1 Renal Neoplasm. Urology. 2017;35(96):453-464.
- Xi W, Wang J, Liu L, et al. Evaluation of tumor pseudocapsule status and its prognostic significance in renal cell carcinoma. J Urol. 2018;199(4):915-920.
- Alhalabi O, Karam JA, Tannir NM. Evolving role of cytoreductive nephrectomy in metastatic renal cell carcinoma of variant histology. Curr Opin Urol, 2019 Sep;29(5)521-525.
- Mejean A, Ravaud A, Thezenas S, et al. Sunitinib alone or after nephrectomy in metastatic renal cell carcinoma. N Engl J Med 2018 Aug 2;379(5):417-427.


