Radical cystectomy is the gold standard treatment for muscle-invasive bladder cancer. However, this treatment has significant limitations, including a high mortality rate of up to 50% within five years from surgery, a high complication rate of up to 67%, a perioperative mortality rate ranging between 1.5-4.5%, urinary incontinence, impaired sexual function, reduced quality of life, and altered body image.
The authors aimed to find an alternative treatment with similar or better oncological results, improved quality of life, and reduced toxicity. Some small retrospective studies published in the past have shown some benefit to brachytherapy in these patients. The authors decided to further explore this alternative therapeutic option and upgrade it in such a way that will result in improved outcomes and preserve their bladders. This alternative approach consisted of maximal transurethral resection of the bladder tumor (TURBT), external beam radiotherapy, and brachytherapy using the advantages of robotic-assisted laparoscopic surgery. For this alternative approach, only patients with clinical stage T1-T3aN0, grade 2-3, with no carcinoma in situ, and tumor size less than 5 cm, were included.
According to the protocol of this trial, all patients underwent a preoperative pelvic MRI. Eight weeks after the TURBT, external beam radiotherapy was administered with 40 Gy in 20 fractions applied to a clinical target volume which included the bladder and the pelvic regional lymph nodes. A week later, a robotic-assisted procedure is performed where brachytherapy catheters are inserted (Figure 1). Through the entire procedure, the surgeons have both a cystoscopic and laparoscopic view of the bladder. Certain conditions mandated the performance of a partial cystectomy. These included when a residual tumor of more than 1 cm was left in a resectable part of the bladder, when a tumor was located inside a diverticulum, or when the distal ureter was involved. Additionally, selective pelvic lymph node dissection was performed in cases with suspicious lymph nodes seen in the preoperative pelvic MRI. Follow-up of these patients was performed with routine cytology and cystoscopy every three months, MRI, and or PET-CT when required.
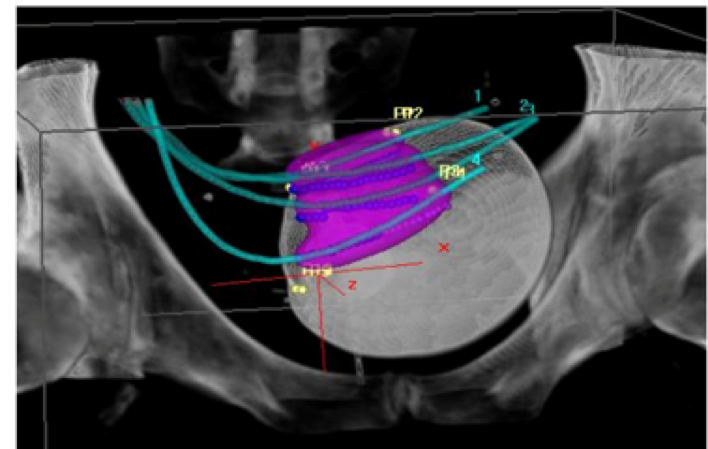
Figure 1 – Brachytherapy catheters inserted using the robotic approach:
Overall, 119 patients were treated in this protocol, with four patients excluded from the final analysis. In 38 patients (33%) partial cystectomy was performed, and 36 patients (31%) pelvic lymph node dissection was performed. The median hospitalization time was five days, and 16 patients (14%) had grade 3 or 4 complications. According to the authors, no change in the functional bladder outcomes or sexual functions were noted by the patients. Mean follow-up time was 2.0 years (1 month-8.8 year). Survival analyses demonstrated that the two-year local control was 82%, and the two year-disease specific survival was 89%. Importantly, no infield recurrences were witnessed in the partial cystectomy patients.
The authors concluded that this alternative minimally invasive therapeutic approach results in excellent oncological and functional outcomes; and can be offered to appropriately selected patients, as a bladder-sparing approach with minimal toxicity. This is a most interesting study showing encouraging results. However, there are some limitations that must be addressed. These include the short follow-up time, the lack of control group undergoing standard radical cystectomy, and the fact that this is a single center experience only. Further exploration of this novel therapeutic approach should be pursued on a larger scale.
Presented by: Smirts Geert and van-der Steen-Banasik EM, Rijnstate Hospital, Arnhem, The Netherlands
Written By: Hanan Goldberg, MD, Urologic Oncology Fellow (SUO), University of Toronto, Princess Margaret Cancer Centre @GoldbergHanan at the Global Conference on Bladder Cancer 2018 - September 20-21, 2018 Madrid, Spain


