RILND has a high morbidity rate of 30-50%, which includes wound infection, skin flap necrosis, lymphocele, lymphedema, deep vein thrombosis/pulmonary embolism, and inner thigh paresthesia. These have severe effects on patient quality of life.
Due to this, there have been several modifications performed to the RILND. These include a modified template, preservation of the great saphenous vein, dissection medial to the femoral artery, performance of supra-inguinal dissection, and utilization of a mini-invasive approach.
Dr. Ayres continued to discuss the clinical N0 stage in the groin region. Approximately 60-70% of invasive penile carcinomas present with impalpable inguinal lymph nodes. However, 20% of patients and 13% of inguinal basins harbor micro-metastatic disease. Unfortunately ultrasound and CT scans do not have the adequate resolution to detect small volume disease. This results in a high rate of overtreatment and morbidity. In order to avoid the morbidity and complications associated with RILND, the dynamic sentinel lymph node biopsy (DSNB) approach has been used. Other methods include increasing the CT scan resolution to 8-10 mm, and to use risk adapted nomograms.
The concept behind DSNB states that there is a stepwise /predictable drainage of the lymph nodes in the inguinal region. It is assumed that the first lymph node in the chain acts as a filter. Therefore, if the sentinel node is clear, the rest of the nodes in the inguinal basin are clear as well. It is important to note that there could be a false positive possible if the node is full of tumor. Usage of DSNB has shown an improvement in survival from 82% between 1956-1993 to 91% between 1994-2012. In the current European Association of Urology (EAU) guidelines DSNB or bilateral modified inguinal lymphadenectomy is recommended in clinical stage N0 and >T1G2.
Recent advances in penile cancer include the development of Eurogen, A European reference network, approved by the European commission, working in a multidisciplinary approach. It presents an online platform to enable expert multidisciplinary review of complex rare cases including penile cancer. It also supports research collaboration and education.
In summary, DSNB for clinical stage N0 penile cancer has good accuracy with false negative rates up to 12%. It significantly reduces morbidity and improves survival. In the future, imaging and tracer advances may improve/refine further. Advanced disease and lymphedema remain a therapeutic challenge.
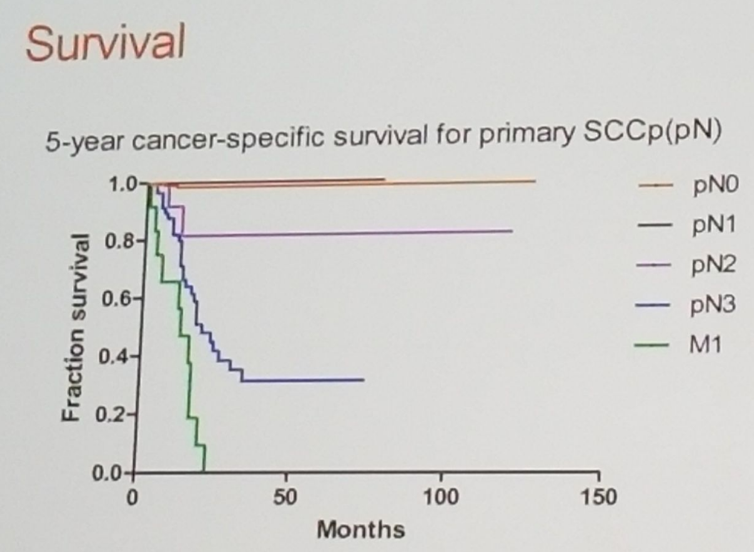
Figure 1: Five year cancer specific survival for Penile cancer stratified by Pn stage:
Speaker: Ben Ayres, MD Royal College of Surgeons, St George’s medical school, St George’s Hospital London, United Kingdom
Written By: Hanan Goldberg, MD, Urologic Oncology Fellow (SUO), University of Toronto, Princess Margaret Cancer Centre @GoldbergHanan at The 15th Meeting of the EAU Section of Oncological Urology ESOU18 - January 26-28, 2018 - Amsterdam, The Netherlands


