Due to significant difficulties in conducting prospective trials attempting to analyze the added benefit of CN to MRCC patients, we are only left with retrospective studies, and registry data. A paper published in the Journal of Clinical Oncology in 2016 tried to retrospectively analyze this question [1]. This was a retrospective analysis of the National cancer database (NCDB) in the US. Overall 15390 patients with Mrcc treated with targeted therapy were analyzed. Two specific analyses were performed:
• To assess predictors of receipt of CN
• To assess effect of CN on overall survival
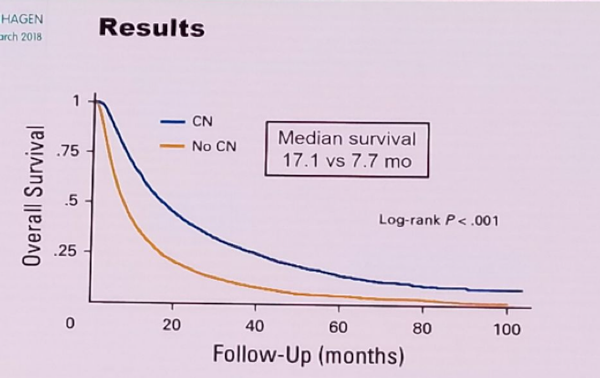
Figure 2 demonstrates the consort diagram of the study. The results showed a clear survival advantage in patients undergoing CN (17.1 vs. 7.7 months) (Figure 3). Multivariable analysis also demonstrated that CN was a significant predictor of improved survival, with a hazard ratio of 0.49, p<0.001. The beneficial effect of CN increased with increasing survival time.
Aside from the obvious retrospective nature of the study with its associated selection bias, the major limitations include lack of data on the prognostic risk factors of the patients, including performance status, and lack of data on the type and duration of the lines of treatment patients received.
Whether this study helps us decide who should and who should not undergo CN is still debatable. Although this study demonstrates that CN has a benefit, in the real-world, CN is done less and less. Data from the SURTIME study demonstrates that the deferred CN approach appears to select out patients with inherent resistance to systemic therapy, who will probably not benefit the from the addition of CN.
In summary, younger male patients, with few comorbidities, with lower T and N stages, with better blood parameters, and better response to targeted therapy will probably benefit the most from CN. Patients who are good responders to targeted systemic therapy, with oligo-metastatic resectable disease, preferably in the lungs only, are the better patients to attempt a CN. CN is probably not very useful in patients with a life expectancy of less than 12 months, with +3-4 negative prognostic factors, who have bulky metastatic load, and who are non-responders to systemic therapy.
Figure 1: Treatment for metastatic Renal cell carcinoma throughout the years:
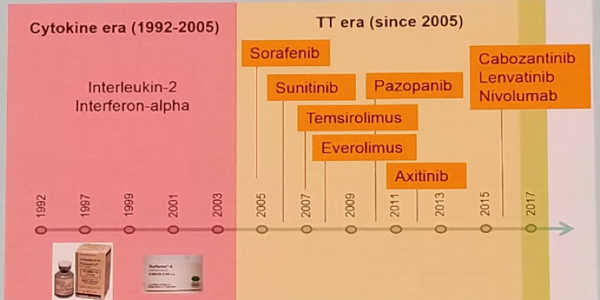
Figure 2 – Consort diagram of the JCO paper assessing the effect of cytoreductive nephrectomy in metastatic RCC patients:
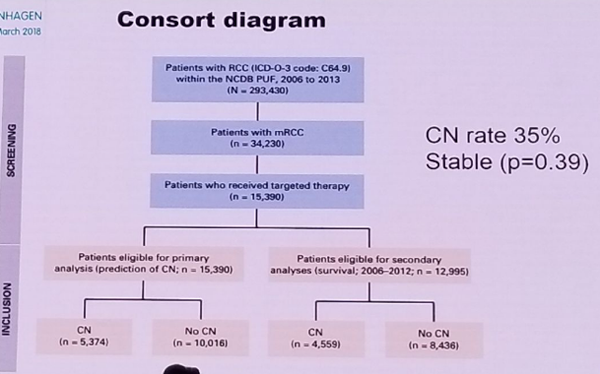
Figure 3: Clear advantage for cytoreductive nephrectomy in overall survival in the JCO paper assessing the effect of cytoreductive nephrectomy in metastatic RCC patients
Speaker: T. Klatte, Cambridge (GB), H. Van Poppel, Leuven (BE)
Written by: Hanan Goldberg, MD, Urologic Oncology Fellow (SUO), University of Toronto, Princess Margaret Cancer Centre, Twitter:@GoldbergHanan, at the 2018 European Association of Urology Meeting EAU18, 16-20 March, 2018 Copenhagen, Denmark


