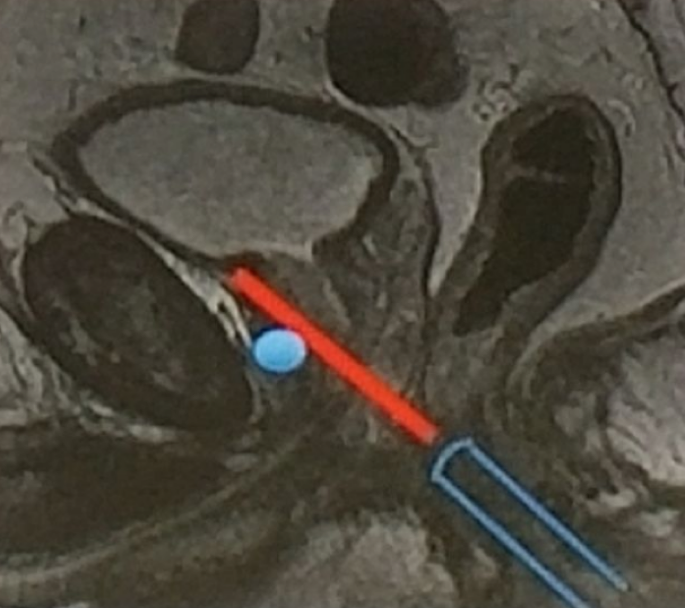
According to Dr. Rouviere, cognitive guidance is simple, quick, and requires no additional hardware. On the contrary, there is potential for human error in extrapolation of the US imaging plane from MRI images. It is imperative for the operator to have a good understanding of the position of the lesion in the prostate to make an accurate biopsy. This can be obtained only by reviewing all MRI images. Relying only on a narrative MR report or even on a schematic diagram is far from satisfactory. The operator must also be aware of systematic biases induced by the fact that so-called “axial” MRI and US images are not obtained along the same plane (Figure 1). Using an end-fire probe, the relative symmetry of the prostate causes axial MRI and US planes to look similar despite large angulation differences which lead to inaccurate targeting. With cognitive guidance, cores targeting posterior lesions tend to be obtained in a plane that is located too close to the apex (Figure 1). Conversely, cores directed at anterior targets tend to err toward the prostate base (Figure 2).
A systematic review of the recent literature compared direct in-bore guidance, software-assisted MRI/US fusion and cognitive guidance. It did not show clear superiority of one technique over the others. [1] Two studies compared cognitive guidance and MRI/US fusion in the same patients. One did not find any difference.[2] The other found a trend for higher tumor detection rates in favor of MRI/US fusion. [3] A major bias disrupting the interpretation of these trials, is that the experience of biopsy operators plays a major role in the precision of targeted biopsies, not only with cognitive guidance , but also with MRI/TRUS fusion.[4]
In summary, cognitive biopsy is fast and free, but requires expertise and rigorous technique. If these conditions are met, the results are satisfactory. However, the accuracy of cognitive biopsy is probably slightly inferior to that of fusion or in-bore biopsy. Dr. Rouviere suggests that cognitive biopsies be used for large lesions and for the rest – fusion or in-bore biopsies.
Figure 1: Missing posterior lesions

Figure 2 – Missing anterior lesions:
Speaker: Professor Olivier Rouvière, MD, PhD, Professor of Radiology Department of Genitourinary and Vascular Radiology Pavillon P Radio, Hôpital E. Herriot Lyon, France
Written By: Hanan Goldberg, MD, Urologic Oncology Fellow (SUO), University of Toronto, Princess Margaret Cancer Centre @GoldbergHanan at The 15th Meeting of the EAU Section of Oncological Urology ESOU18 - January 26-28, 2018 - Amsterdam, The Netherlands
References:
1. Wegelin O, van Melick HH, Hooft L, et al. Comparing Three Different Techniques for Magnetic Resonance Imaging-targeted Prostate Biopsies: A Systematic Review of In-bore versus Magnetic Resonance Imaging-transrectal Ultrasound fusion versus Cognitive Registration. Is There a Preferred Technique? Eur Urol 2017;71:517-31.
2. Puech P, Rouviere O, Renard-Penna R, et al. Prostate Cancer Diagnosis: Multiparametric MRtargeted Biopsy with Cognitive and Transrectal US-MR Fusion Guidance versus Systematic Biopsy--Prospective Multicenter Study. Radiology 2013;268:461-9.
3. Wysock JS, Rosenkrantz AB, Huang WC, et al. A prospective, blinded comparison of magnetic resonance (MR) imaging-ultrasound fusion and visual estimation in the performance of MRtargeted prostate biopsy: the PROFUS trial. Eur Urol 2014;66:343-51.
4. Moldovan P, Udrescu C, Ravier E, et al. Accuracy of Elastic Fusion of Prostate Magnetic Resonance and Transrectal Ultrasound Images under Routine Conditions: A Prospective MultiOperator Study. PloS one 2016;11:e0169120.


